
Gå tillbaka
Diabetes and Metabolic Risk in mental illness
Från SFDs vårmöte i maj 2007.
Abstract
Diabetes and cardiovascular disease
is increased 2-3 fold in people with schizophrenia. Furthermore there is a high
prevalence of undiagnosed metabolic disease in people with schizophrenia. The
reason for this increase is multifactorial and therefore there is a need to assess
and manage diabetes and cardiovascular risk factors in all individuals with schizophrenia.
Despite increased interest in the physical health consequences of schizophrenia,
monitoring of diabetes and cardiovascular risk factors remains poor.
Screening
for diabetes and cardiovascular risk factors should be undertaken annually. Lifestyle
programmes should be instituted to reduce the risk of diabetes and cardiovascular
disease. Group sessions to address overweight and obesity are at least as effective
as in the general population. People with schizophrenia should not be denied pharmacological
interventions to reduce cardiovascular disease because of their mental illness.
Closer liaison is needed between physical and mental health services to improve
the health outcomes of people with schizophrenia.
Introduction
Over the last 5 years, there has been an increasing awareness of the physical
health needs of people with severe mental illness. Schizophrenia is associated
with a 2-3 fold increased risk of premature mortality and the life expectancy
of people with severe mental illness is shortened by 10-20 years [1]. Although
the highest relative risk of mortality is associated with suicide and trauma,
three quarters of all deaths in people with severe mental illness are secondary
to physical illness, with cardiovascular disease accounting for the highest number
of deaths.
The management of physical health of people with severe mental
illness require a close collaboration between psychiatric and physical health
services to ensure that this vulnerable patient group has access to the best health
care. In May 2007, the Swedish Society for Diabetology organised a joint symposium
for diabetologists and psychiatrists to gain a greater understanding of the problem
and to develop care pathways to address the physical health needs of those with
mental illness.
This meeting was timely because many working within physical
health services have been unaware of the increased mortality and morbidity of
people with mental illness until recently. This can be understood when it is appreciated
that the overall prevalence of severe mental illness is around 1%. Given that
diabetes and cardiovascular disease is increased 2-3 fold in people with severe
mental illness, it would be expected that only around 3% of patients attending
for physical health services would have a mental illness [2]. Given the difficulties
that people with mental illness have in accessing these services, the figure of
3% may rapidly fall back to 1% or even less, at which point the excess burden
of physical disease would not be appreciated by those working outside psychiatric
settings [3]. This paper is based on my lecture at this meeting.
Prevalence
of Diabetes and Metabolic Syndrome
Although the association between
diabetes and schizophrenia has been recognised for over a century, precise prevalence
rates of diabetes are difficult to obtain [2]. This partly reflects the rapid
change in prevalence within the general population but also results from the much
higher rates of undiagnosed diabetes in people with mental illness and their reluctance
to take part in epidemiological studies. Nevertheless despite these difficulties,
the literature is consistent in showing a 2-3 fold increase in diabetes giving
an overall prevalence of ~10-15% in Western developed countries [4-11]. The greatest
excess risk appears to occur in younger adults suggesting that diabetes is being
accelerated by 10-20 years [8].
The pattern is very similar for prevalence
rates of metabolic syndrome which again are increased 2-3 fold, with the greatest
excess in those aged 20-40 years old [12-23]. It is worth bearing in mind that
only around 15% of people with schizophrenia have no features of metabolic syndrome
with central obesity being the commonest problem [19].
Coronary heart disease
mortality is increased 1.9 - 3.2 fold in those with severe mental illness, with
the largest increase being seen in those under the age of 50 years. Similarly
stroke mortality is increased 1.3 – 2.5 fold [24].
Screening
for Diabetes and Metabolic Problems
It is well recognised that diabetes
and other metabolic problems are frequently asymptomatic [25]. It is estimated
that within the general population, the onset of diabetes precedes diagnosis by
around a decade, although there is now evidence based on glycosylated haemoglobin
at diagnosis that people are being diagnosed earlier. During this asymptomatic
period, patients are at risk of macrovascular and microvascular complications
of diabetes. Consequently diabetes is frequently diagnosed following a cardiovascular
event and over 50% of people with newly diagnosed diabetes in the UK Prospective
Diabetes Study had microvascular complications [26,27]. This observation places
a strong imperative for screening the general population but it is even more crucial
for those with severe mental illness where the rates of both diagnosed and undiagnosed
are higher [11,28]. For this reason, several diabetes associations, including
Diabetes UK and the Canadian Diabetes Association have recommended routine screening
in those with severe mental illness.
Local agreement is needed to ensure
that it is clear who has the responsibility for screening. The UK National Institute
for Clinical Excellence places the primary responsibility within primary care
but secondary care psychiatry services are encouraged to undertake regular assessment
of physical health and should assume responsibility if patient does not see their
general practitioner. This should mean that all are screened but in practice many
patients fall between both services and are not screened.
Obtaining fasting
blood samples in people with severe mental illness can be challenging and as the
sensitivity and specificity for fasting and random samples for the diagnosis of
diabetes are similar, the pragmatic approach would be to obtain a fasting sample
where possible but a random sample is a reasonable alternative where a fasting
sample is not feasible and certainly better than no sample at all [29]. Patients
should be screened prior to starting or switching antipsychotic medication, 3-4
months later (to detect the few patients who develop diabetes rapidly following
treatment with an antipsychotic) and then annually.
Diabetes Prevention
One of the most exciting areas in diabetes at present is the possibility
that it can be prevented by lifestyle modification. Studies from Finland, China
and the USA have demonstrated that modest weight loss in association with dietary
changes to increase fibre while at the same time reducing fat, in particular saturated
fat, and 30 minutes of exercise can reduce incident diabetes by nearly two-thirds
in high risk individuals over a 3 year period [30,30-32]. The challenge has been
to implement these trial findings in routine clinical practice and this also applies
to people with severe mental illness. For too long, there have been feelings of
therapeutic nihilism that have prevented healthy lifestyle programmes from being
offered to people with severe mental illness.
Recently studies have shown
that this pessimism has been misplaced [33,34]. Weight loss and lifestyle modification
is possible; one example is the Salford weight management clinic, which achieved
a mean weight loss of 7% in self selected people with severe mental illness after
a year (figure 1) [34]. The Salford clinic operates a weekly group session during
which the patients are educated about healthy living and are invited to make stepwise
changes to their lifestyle. There is plenty of opportunity for change: some patients
describe drinking 10 litres of sugary carbonated beverages daily and so switching
to diet drinks or water can significantly reduce sugar and calorie intake. The
challenge to health care professional is to ensure that these healthy messages
are conveyed to people with severe mental illness as it is likely that they have
not heard these before.
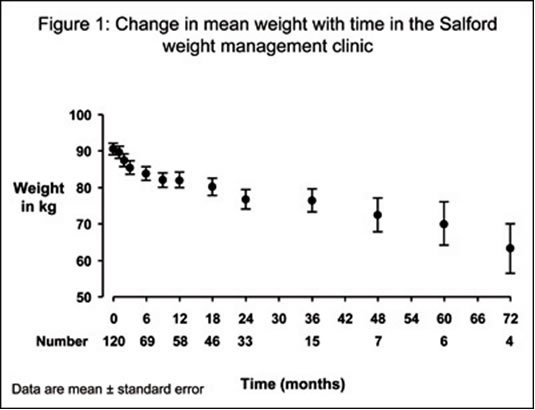
Figure 1: Change in mean weight with time in the Salford weight management
clinic.
Pendlebury et al Presented at Society of Biological Psychiatry
2007
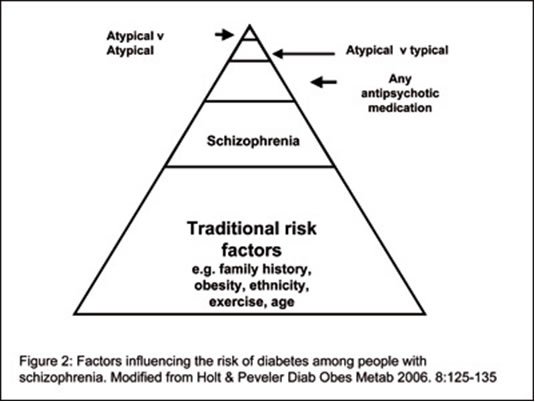
Figure 2: Factors influencing the risk of diabetes among people with
schizophrenia.
Modified from Holt & Peveler Diab Obes Metab
2006. 8:125-135
How to manage diabetes?
Diabetes is a complex chronic condition that requires the patient to take multiple
medications and adopt healthy lifestyle choices. Diabetes education is needed
to empower the patient to take control of their diabetes for the vast majority
of the time when they do not have access to health care professionals. These principles
also apply equally to people with severe mental illness and therefore the diabetes
should be managed by someone with suitable expertise in diabetes management.
People with severe mental illness, however, have additional needs and therefore
there needs to be a close collaboration between psychiatric and diabetes services.
First and foremost is the need to treat the psychotic state because without this,
diabetes education is likely to be futile!
There has been considerable discussion
about the role of antipsychotic drugs in the development of diabetes in people
with severe mental illness and there are arguments about whether the antipsychotic
should be stopped if a patient develops diabetes or whether certain antipsychotics
should be avoided in patients with diabetes or who are at high risk of diabetes.
These arguments appear misplaced because the aetiology of diabetes in people with
mental illness is multifactorial (figure 2), as it is in the general population
and the role of the antipsychotic drugs is small [35].
Both genetic and environmental
risk factors account for the increase in diabetes. Between 17-50% of people with
schizophrenia have a family history of diabetes and examination of the genome
reveals hot-spots that are common for both conditions [36,37]. Low birth weight
is associated with a higher prevalence of diabetes and schizophrenia in later
life suggesting that a common insult in early life may predispose the individual
to both diseases [38].
The adult lifestyle of people with mental illness
plays a pivotal role. As intimated before, people with schizophrenia have diets
that are rich in saturated fat and refined sugars while being poor in fruit and
vegetables [1,39]. They are less physically active and have high prevalence rates
of smoking. The illness of schizophrenia itself may increase the risk of diabetes;
some but not all studies of first episode patients have demonstrated increased
insulin resistance, impaired fasting glycaemia and central obesity compared with
well matched controls [40-43]. One possible mechanism is hypercortisolaemia and
increased catecholamine secretion which is a feature of psychosis [44]. Interestingly
in one study, treatment of an acute episode of psychosis was associated with improvements
of both islet cell function and insulin secretion [45].
While antipsychotic
drugs are undoubtedly the cause of diabetes in a small number of cases, larger
studies have not shown a consistent difference between antipsychotics and placebo
or between individual drugs [35]. Almost certainly the reason for this is the
complex interaction between drug, patient and environment. To illustrate this,
consider the patient receiving drug A which has a higher risk of diabetes than
drug B, based on cell and animal studies. If drug A is more effective in treating
the psychosis for that patient and the patient is then more able to undertake
lifestyle modification, then any pure pharmacological differences may be completely
swamped by differences in traditional environmental risk factors.
There are
two themes that emerge from the observational studies: first that treatment with
any antipsychotic is associated with more diabetes than no antipsychotic and secondly
that in general treatment with an atypical antipsychotic is associated with more
diabetes than a conventional agent [35]. When studies compare different atypical
drugs, the picture is much less consistent, with some studies showing higher risks
for some drugs, while others show the opposite.
Part of these differences
can be explained by the methodology used in these studies and three main flaws:
treatment assignment bias, screening bias and inadequate adjustment for major
confounders [35]. The studies are not randomised and therefore any differences
in diabetes may have resulted from other non-drug related factors. For example,
clozapine, which is reserved for treatment resistant patients, is associated with
the highest rates of diabetes, which could have occurred because these individuals
were at highest risk because of the severity of their illness. Patients receiving
atypical drugs are screened more frequently than those receiving conventional
agents and inevitably more cases of undiagnosed diabetes will be found through
this screening [46].
Most observational studies are undertaken by interrogating
large databases to determine how many people receiving an antipsychotic at baseline
begin diabetic treatment over a fixed period of time. As well as ignoring those
treated with lifestyle modification alone, the databases do not provide information
on important diabetic risk factors such as obesity, family history or lifestyle.
Added to these three sources of bias is publication bias, where the results of
studies sponsored by the pharmaceutical industry are generally in favour of their
own drug [47].
Even allowing for these methodological problems, it is clear
from the observational studies that the risk of developing diabetes with the antipsychotics
is low. All studies show that the attributable risk of the antipsychotics is less
than 5% meaning that most individuals treated with antipsychotics will not develop
diabetes as a result of their treatment [48].
In addition to the observational
studies, there are around 20 prospective trials that have reported glucose abnormalities
with antipsychotics and none have shown differences between antipsychotics or
indeed between drug and placebo despite quite marked differences in weight gain.
While these data are encouraging, some caution is needed because these studies
are underpowered to detect metabolic abnormalities and reporting of such abnormalities
is of variable quality. Most studies are less than 1 year in duration and do not
study drug naïve subjects [35].
With this in mind, should the antipsychotic
drug be stopped if a patient develops diabetes? Where it is clear that the diabetes
has developed rapidly following the initiation of treatment, the answer is probably
yes but this should be balanced with the psychiatric needs of the patients. In
most other cases, however, the drug should not be stopped. Consider the following
case history: a 45 year old man with schizophrenia was an in-patient at a high
security hospital because of a violent history. During his admission he had been
well, both physically and mentally as a result of treatment with an atypical antipsychotic,
before he developed diabetes 7 years later. The psychiatrist was concerned about
the side-effects of the antipsychotic and switched him to another atypical agent.
The man had a psychotic relapse and nearly murdered a fellow patient but his diabetes
did not resolve.
We should not be surprised by this outcome because the
underlying aetiology of diabetes in this man was not likely to be the antipsychotic
and there is always a risk of relapse if medication changes are made.
The
reason why the man was receiving the antipsychotic was his mental illness and
this should be the first and foremost priority for his health care professional
team. Consider the parallel with a patient with asthma and diabetes. During an
acute asthmatic attack, the most appropriate treatment is corticosteroid despite
its adverse effect on glucose metabolism as the asthma is the patient’s
overriding problem. The same is also true for patients with psychosis and diabetes
except the risk of worsening diabetes with the antipsychotic is much smaller:
the overriding problem is the psychosis and this requires urgent treatment. Indeed
treatment of the mental illness is a prerequisite for the management of the diabetes.
For these reasons, the choice of antipsychotic and timing of discontinuation
should be primarily driven by efficacy rather than concerns about side effects.
How to manage cardiovascular risk?
The increase in
features of the metabolic syndrome and other cardiovascular risk factors in people
with severe mental illness places a need on health care professionals to screen
and treat these in order to reduce the burden of cardiovascular disease in this
patient population [49]. In addition to diabetes, traditional cardiovascular risk
factors should be screened on an annual basis (table 1).
The individual’s
overall cardiovascular risk can then be calculated using conventional risk engines.
Although these are likely to underestimate the risk, there are no specific risk
engines for people with severe mental illness and so the available general population
models provide the best estimate.
Many of the principles of cardiovascular
disease prevention run in parallel to diabetes prevention. Patients should be
encouraged to adopt a healthy lifestyle and as for diabetes, this will require
treatment of the mental illness to allow the patient the capacity to make healthy
lifestyle choices. Where cardiovascular disease prevention differs from diabetes
prevention is the well established use of pharmacotherapy to prevent diabetes.
There is no evidence that these medications are less effective in people with
mental illness and therefore should be used as for the general population. As
compliance may be challenging in this group of patients, additional time and support
may be needed to ensure that the patient understands the need for the treatment.
Conclusion
People with severe mental illness have an increased prevalence of both diabetes
and other features of the metabolic syndrome that increase the subsequent risk
of cardiovascular disease. As these are asymptomatic, it is the responsibility
of the health care professionals caring for those individuals to screen and manage
them appropriately. Treating the mental illness is essential to the successful
management of diabetes and cardiovascular risk factors and therefore there needs
to be close liaison between health care professionals working in physical health
and psychiatric settings to enable the person with mental illness can achieve
a long and healthy life.
Duality of Interest: Richard IG Holt has received
educational grants and fees for lecturing and consultancy work from Eli Lilly
and Company, Bristol Myers Squibb and GlaxoSmithKline. Dr Holt did not receive
any payment by any pharmaceutical company for the writing of this report.
Dr
Richard IG Holt
Institute of Developmental Sciences Building
(MP887)
Southampton General Hospital
Tremona Road
Southampton SO16 6YD, UK
Tel: +44 23 8079 4665
Fax:
+44 23 8079 4945
|Upp|
