Sammanfattningar
- ACE-I may be protective beyond BP
control in diabetic patients
- Diabetes diagnosis prompts smokers
to quit
- Learning to cope has lasting benefits
in young diabetics
- Insulin glargine provides better
glucose control than NPH insulin
- Rökning och snus medför risk för
typ 2 diabetes
- Inhaled insulin as effective as
injections
- Hyperlipidemia treatment
in diabetics is cost-effective
- Intensive blood glucose control
is cost-effective in type 2 diabetics
- New TZD shows potent antidiabetic
properties in mice
- TZDs prevent glomerular dysfunction
in diabetic rats
- Nytt från UKPDS
- Många patienter tar inte sin ordinerade
medicin
- Sildenafil reverses diabetic
gastroparesis in mice
- Det metabola syndromet är relaterat
till tjocka vänsterkammar-väggar
men inte till vänsterkammar-hypertrofi
- Referenser
upp
ACE-I may be protective
beyond BP control in
diabetic patients
Från Diabetes Care
2000;23:882-883,888-892.A meta-analysis of four trials, in which patients with hypertension and type 2 diabetes were randomized to receive ACE inhibitors or a different drug, shows that ACE inhibitors provide particular advantages over and above control of blood pressure. Dr. Marco Pahor, of Wake Forest University Baptist Medical Center, Winston-Salem, North Carolina, and colleagues collected data on 470 subjects in The Appropriate Blood Pressure Control in Diabetes trial, which compared enalapril with nisoldipine.
Also studied were 572 subjects in the Captopril Preven-tion Project, which compared captopril with diuretics or beta-blockers; 380 patients in the Fosinopril Versus Amlodipine Cardiovascular Events Trial, which compared fosinopril with amlodipine; and 758 subjects in the UK Prospective Diabetes Study, which compared captopril with atenolol. The results are published in the July issue of Diabetes Care. Dr. Pahor’s team found that ”the cumulative results of the first three trials showed a significant benefit of ACE inhibitors compared with alternative treatments on the outcomes of acute myocardial infarction (63% reduction), cardiovascular events (51% reduction) and all-cause mortality (62% reduction),” according to the researchers.
These advantages were not found in the last trial, where the ”question of whether atenolol is equivalent to captopril remains open,” according to the report. Co-investigator Dr. Michael H. Alderman, of Albert Einstein College of Medicine, Bronx, New York, told Reuters Health that ACE inhibitors are as protective in the general population, ”but diabetics are at higher risk and so with the same relative benefit you get a bigger bang for your buck.” Citing the Heart Outcomes Prevention Evaluation (HOPE) study, Dr. Alderman said, ”There is evidence that ACE inhibitors will be useful in all diabetics, not just hypertensives.”
In a related editorial Dr. Hertzel C. Gerstein, of McMaster University, Hamilton, Ontario, Canada, writes, ”These data support the recommended use of ACE inhibitors as first-line agents in people with diabetes who are at a particularly high risk for cardiovascular outcomes.” He adds, ”Furthermore, they suggest that ACE inhibitors should be used as firstline anti-hypertensive agents in all people with diabetes.”
upp
Diabetes diagnosis prompts
smokers to quit
SAN ANTONIO, Jun 15 (Reuters Health)
- Being diagnosed with diabetes increases the likelihood that a smoker will quit smoking, according to a researcher from the University of Michigan, Ann Arbor. In an earlier study, Dr. Linda A. Wray and colleagues reported that people with acute MI were seven times more likely to quit smoking than people who had not had a heart attack.
”I would like to think that the public health information that’s out there would be enough to prompt people to quit smoking before they’re diagnosed with diabetes or a heart attack,” Dr. Wray told Reuters Health. ”In fact it does for a lot of people, but there are some people that clearly it takes something that serious before they do finally quit smoking.”
As described in a poster presented here at the annual meeting of the American Diabetes Association, she studied a group of 1,945 middle-aged smokers who were part of the Health and Retirement Study and who were smoking in 1992. Of this group, 345 quit smoking by 1996, and 33 were diagnosed with type 2 diabetes by 1994. Even though this group was heavily addicted to smoking, Dr. Wray found that the group diagnosed with diabetes was still 2.4 times more likely to have quit smoking by 1996.Socioeconomic status or ethnic background did not predict whether a smoker would quit after a diabetes diagnosis. ”Because they are sort of a special group of smokers, I think it also suggests that maybe a ’one-size fitsall’ kind of smoking cessation program doesn’t always work,” she said. ”Sometimes you need more, you need different kinds of techniques depending on who the target audience is.”
upp
Learning to cope has lasting benefits in young diabetics
Från J Pediatr
2000;137:107-113.The success of intensive therapy regimens in young people with diabetes mellitus appears to be increased by training in coping skills, researchers report in the July issue of The Journal of Pediatrics. Dr. Margaret Grey, of Yale University School of Nursing, New Haven, Connecticut, and colleagues note that ”adolescence is a particularly difficult time to achieve nearnormal blood glucose values.” To determine if enhanced coping skills would be helpful in improving metabolic control, the researchers randomly assigned 77 patients, ages 12 to 20 years, who were about to begin intensive diabetes management, to intervention or control groups. Intervention patients attended six training sessions in groups of two or three and were followed up monthly.
Emphasis was placed on developing skills in areas such as social problem solving, cognitive behavior modification and conflict resolution. Clinical data were collected monthly and subjects were assessed at 3, 6 and 12 months after the intervention by means of a variety of scales covering psychological and other factors. Although both groups were comparable at baseline, after 1 year, intervention patients had lower glycosylated hemoglobin and achieved better diabetes and medical selfefficacy scores. In addition, diabetes had less impact on their quality of life. The intervention also decreased the incidence of weight gain and hypoglycemia in females, but not in males. Given these findings, the researchers conclude that ”the addition of behavioral intervention to intensive diabetes management in adolescence results in improved metabolic control and quality of life over 1 year.”
upp
Insulin glargine provides better
glucose control than NPH insulin
Från Diabetes Care
2000;23:1130-1142.In patients with type 1 or type 2 diabetes, single daily injections of insulin glargine provide glucose control superior to that afforded by once or twice-daily NPH insulin administration, according to two reports in the August issue of Diabetes Care. Insulin glargine is a recombinant human insulin analog designed to have a smooth, peakless profile of action when injected subcutaneously, the authors explain. Dr. Hannele Yki-Jarvinen, of the University of Helsinki, Finland, and colleagues compared insulin glargine with NPH insulin in the treatment of 426 patients with type 2 diabetes poorly controlled with oral hypoglycemic drugs.
Insulin doses, C-peptide concentrations and hemoglobin A1c levels did not differ between the two treatment groups, the authors report. Diurnal glucose profiles differed significantly, however, with insulin glarginetreated patients demonstrating lower blood glucose concentrations both before and after dinner. Furthermore, 3:00 AM blood glucose levels among patients achieving their fasting blood glucose targets were lower with NPH insulin than with insulin glargine treatment. Significantly more patients treated with NPH insulin experienced symptomatic hypoglycemia than did insulin glargine treated patients, the investigators note.
”These data support use of insulin glargine instead of NPH in insulin combination regimens in type 2 diabetes,” the authors conclude. Dr. Julio Rosenstock and colleagues from Dallas Diabetes and Endocrine Center, in Texas, conducted a similar study in 256 patients with type 1 diabetes who were treated with multiple daily insulin regimens. Insulin glargine lowered fasting plasma glucose (FPG) levels to a greater extent than did NPH insulin (9.2 mmol/L versus 11.3 mmol/L, respectively), the authors report.According to the results, FPG levels improved in insulin glargine-treated patients during the study, whereas levels improved in NPH-treated patients only if they had used a once daily regi-men. Like the patients with type 2 diabetes, type 1 diabetics treated with insulin glargine had higher 3:00 AM glucose levels and fewer hypoglycemic episodes than did NPH insulin treated patients, the investigators note. Overall, insulin glarginetreated patients required six to seven fewer units of insulin than did NPH insulin-treated patients. No meaningful differences in adverse events between the two treatments were noted in either study.
upp
Rökning och snus medför
risk för typ 2 diabetes
Från Medicallinks
nyhetsbrev 11/8 2000.Kära läsare!
Att rökning är en viktig riskfaktor för hjärt/kärlsjukdom är välkänt. Rökning ökar också risken för typ 2-diabetes. En svensk studie, publicerad i augustinumret av Journal of Internal Medicine, visar att rökning av 25 cigaretter eller mer per dag ökar risken 2.6 gånger.Denna studie har under den gångna veckan funnits på Medical Links förstasida. Om man hade diabetes i släkten sexdubblades risken! En japansk studie visar att män som röker minst 31 cigaretter per dag fyrdubblar risken för typ 2-diabetes. Gunilla Bolinder vid KS har visat att snusning ökar risken för hjärt/kärlsjukdom mindre än rökning. Hon har också visat att rökning, men inte snusning, ökade omfattningen av ateroskleros i halskärlen mätt med ultraljud.
Den nu aktuella svenska studien visar att användande av tre dosor snus eller mer per vecka ökar risken för typ 2-diabetes 2.7 gånger. Den bakomliggande mekanismen är oklar. Flera andra forskningsgrupper har visat att nikotintillförsel i form av nikotintuggummin! eller snus leder till ökad insulinresistens, en viktig hörnsten i uppkomst av typ 2-diabetes.
Red
upp
Inhaled insulin as effective
as injections
Från Endocrine Society
Meeting USA summer 2000.Results of a multicenter phase II study show that insulin in a formulation that can be inhaled results in glycemic control comparable to that achieved with conventional subcutaneous administration. The findings were presented by Dr. William Cefalu, of the University of Vermont, at the 82nd annual meeting of the Endocrine Society. He also announced that recruitment has already begun for a large phase III trial using inhaled insulin. A total of 70 patients with type 1 and type 2 diabetes at nine centers were randomized in an open label study to use either the inhaled insulin before meals, with an insulin injection at bedtime, or their usual subcutaneous injections or oral hypoglycemic medication.
There was a 4-week lead-in period to the study, then a 12-week treatment period. Both groups performed home glucose monitoring four times daily, had weekly insulin dose adjustment, and had preprandial glucose targets of 100 mg/dL to 160 mg/dL. The inhalation device comprises a clear plastic cylinder about 10 inches tall, the base of which holds a container of compressed air.
Insulin is kept in small, single dose sachets that are inserted into the device, punctured, and then aerosolized by the compressed air. The patient inhales once through a mouthpiece. Each sachet contains either 1 mg or 3 mg of drug, with the 1 mg sachet being comparable to a 3-unit dose delivered by syringe, Dr. Cefalu said. It was found that the inhaled insulin ”worked similarly well as subcutaneous injections,” he said. It even proved to have an advantage when used in patients with type 2 diabetes who had been on oral agents only.Från Medical Reuters.
upp
Hyperlipidemia treatment in
diabetics is cost-effective
Från Circulation 2000;102:722-727.Treating hyperlipidemia in diabetics is just as effective and cost effective as treating hyperlipidemia in persons without diabetes, according to a report in the August 15th issue of Circulation: Journal of the Ameri can Heart Association. Using the Cardiovascular Life Expectancy Model, Dr. Steven A. Grover and colleagues from The Montreal General Hospital, Quebec, Canada, developed simulations for men and women 40 to 70 years of age. These hypothetical diabetic subjects had pretreatment LDL cholesterol levels of 5.46, 4.34 and 3.85 mmol/L.
The team used 1996 dollars to forecast the long-term costs of cardiovascular events and the need for medical and surgical intervention in this cohort. Comparing their model with data from the Scandinavian Simvastatin Survival Study, Dr. Grover’s group found that ”treatment with simvastatin for patients with cardiovascular disease is cost-effective for men and women, with or without diabetes.”In addition, they noted that ”among diabetic individuals without cardiovascular disease, the benefits of primary prevention were also substantial and the cost effectiveness ratios attractive across a wide range of assumptions (approximately $4,000 to $40,000 per year of life saved).”The findings were also ”robust even among diabetics with lower baseline LDL values and smaller LDL reductions as observed in the Cholesterol and Recruitment Events (CARE) trial.” Dr. Grover and colleagues conclude that ”even in the absence of diagnosed cardiovascular disease or other risk factors, the forecasted longterm benefits of treating hyperlipidemia appear substantial and the costeffectiveness ratios represent good value.”
upp
Intensive blood glucose control is
cost-effective in type 2 diabetics
Från BMJ 2000;320:1373- 1378.Intensive blood glucose control in type 2 diabetics costs more than conventional therapy, but provides savings in the form of reduced complications, according to a report in the May 20th issue of the British Medical Journal. Dr. Alastair Gray, of the University of Oxford, in Headington, UK, and colleagues used data from the 10-year United Kingdom Prospective Diabetes Study to evaluate the cost effectiveness of intensive blood glucose control (maintaining fasting blood glucose below 6 mmol/L) compared with conventional control (maintaining fastingblood glucose below 15 mmol/L) in 3,867 patients with newly diagnosed type 2 diabetes.
The intensive blood glucose control patients received either insulin or sulfonylurea drugs. The average incremental cost of intensive antidiabetic treatment, compared with conventional management, was 659 British pounds sterling, the authors report. In contrast, the mean cost of hospital admissions was higher for the conventional management group (4,266 pounds versus 3,494 pounds for the intensive control group), largely because of longer lengths of stay and slightly higher numbers of admissions.
The reduced cost of complications (hospitalizations) in the intensive control group counterbalanced the increased cost of treatment, the investigators note, resulting in insignificant differences in total costs between the two treatment approaches. These comparisons held when insulin and sulfonylurea therapies were analyzed separately. Cost-effectiveness was evaluated using the incremental cost per year of event-free survival, the report indicates. Discounting the costs at 6% per year and leaving the effects undiscounted, the authors arrive at a cost of 563 pounds per event free year gained.
”With costs and effects discounted at 6% a year,” they add, ”there is a 10% probability that intensive blood glucose control policy would prove to be cost saving compared with a conventional policy, a 50% probability that the cost per event free year lies above (or below) the point estimate of 1,166 pounds, and an 80% probability that the ratio is less than 2,500 pounds.” ”Our results suggest that intensive management of patients with type 2 diabetes is a feasible and economically supportable option,” the authors conclude.Artikeln kan läsas i fulltext
Online: http://www.bmj.com/cgi/ content/full/320/7246/1373
upp
New TZD shows potent antidiabetic properties in mice
Från Diabetes 2000;49:759- 767.NC-2100, a new thiazolidinedione (TZD), controls diabetes without increasing body weight in a mouse model, according to a report in the May issue of Diabetes. A variety of TZDs activate the transcriptional factor peroxisome proliferator activated receptor-gamma (PPAR-gamma) and have potent antidiabetic properties, but they also promote adipogenesis.
Other studies have suggested a relationship between PPAR-gamma activation and both antidiabetic activity and adipogenesis, the authors explain. Dr. Kiyoto Motojima, of Toho University, in Chiba, Japan, and colleagues examined the effects of NC-2100 and other TZDs on plasma glucose, PPAR-gamma activation, and adipogenesis in obese KKAy mice. NC-2100 activated PPAR-gamma much more weakly than did other TZDs, the authors report, and NC-2100 stimulation of adipocyte differentiation was 30 fold weaker than that induced by troglitazone or pioglitazone.
Nevertheless, NC-2100 at concentrations of 0.1% lowered plasma glucose levels as effectively as did 0.1% troglitazone and 0.03% pioglitazone, the results indicate. ”These results strongly suggest that TZD-induced activation of PPAR-gamma does not directly correlate with antidiabetic (glucose-lowering) action,” the authors propose. NC-2100 had little impact on body weight and fat mass, the investigators note, even though it stimulated food intake by 20% to 30%. The increased intake without a concomitant body weight or fat weight increase may be partly explained by NC-2100’s induction of the expression of UCP1, a protein that uncouples proton movement and ATP synthesis and thereby stimulates energy expenditure.
”Interestingly,” the researchers note, ”UCP1 mRNA was induced both in mesenteric and subcutaneous white adipose tissue by NC-2100 in a dose-dependent manner.”
”These characteristics of NC-2100 should be beneficial for humans with limited amounts of brown adipose tissue,” the authors conclude.
upp
TZDs prevent glomerular
dysfunction in diabetic rats
Från Diabetes 2000;49:1022-1032.Japanese researchers have discovered that glomerular dysfunction in diabetic rats is prevented by thiazolidinedione (TZD) compounds, independent of their insulin-sensitizing effects. According to a report published in the June issue of Diabetes, these findings suggest that TZD compounds may have a therapeutic role in diabetic nephropathy.
Dr. Masakazu Haneda and colleagues from Shiga University of Medical Science explain that several in vitro and in vivo studies have suggested that the TZD agent troglitazone may prevent early and late glomerular dysfunction by inhibiting the activation of the diacylglycerol-protein kinase C-extracellular signal-regulated kinase (DAG-PKC- ERK) signal transduction pathway. In the present study, the authors tested this hypothesis by determining whether troglitazone could prevent glomerular dysfunction in rats with streptozotocin-induced diabetes. The investigators report that troglitazone prevented both glomerular hyperfiltration and albuminuria in the diabetic rats.
They also found that this agent increased expression of ECM proteins components of the glomerular mesangium and transforming growth factor beta-1, which is thought to stimulate ECM overproduction. According to the paper, troglitazone abrogated activation of the DAG-PKC-ERK pathway in rat glomeruli independently of its insulin-sensitizing activity. In vitro studies with troglitazone and another related compound, pioglitazone, confirmed these observations.
In light of their findings, Dr. Haneda’s team concludes that ”TZDs might be useful for the prevention of the development and progression of diabetic nephropathy in subjects with type 2 diabetes, by improving metabolic control, and subjects with both types 1 and 2 diabetes, by preventing the activation of the DAG-PKC-ERK pathway.”
upp
Nytt från UKPDS
Rury Holman, UKPDS, angav följande nya sammanfat-tande utdata i juni i Amsterdam vid European Society of Cardiology - se också BMJ online fulltext www.bmj.com 12/8-2000.
Risk för hjärtinfarkt och cerebovaskulär sjukdom: * 14% minskning per 1% minsk-ning i mean HbA1c. 100% av diabetikerna har enligt definition hyperglykemi * 13% minskning per 10 mm Hg minskning i mean systoliskt blodtryck. 50% av våra diabetiker typ 2 har behov av behandling av sitt blodtryck. * 29% minskning per 1 mmol/L minskning i mean LDL-kolesterol. 30-70% av våra diabetiker typ 2 har behoav av lipidsänkande behandling. * 9% minskning per 1 mmol/L stegring i mean HDL-kolesterol. Således bör patienter med typ 2 diabetes få tillgång till en multipel riskfaktorkontroll för man skall lyckas med prevention av makrovaskulär sjukdom.
Red
upp
Många patienter tar inte
sin ordinerade medicin
Mats Foldevi, allmänläkare och lektor vid Linköpings univer-sitet har gjort en forskningsrapport i ämnet. Språkproblem förekom mer som en orsak. Vi måste lära oss att bemöta också patienter som har information via internet, de köper inte ett argument bara för att jag säger det. En mer engagerad patient är en nyckelfaktor för en lyckad behandling, anser Foldevi. Följer patienten läkemedelsordinationen? Svaret är ”nej” i nästan sju fall av tio. Vid mellan hälften och en tredjedel av alla läkemedelsordinationer tar patienten medicin enligt ordination.I en terdjedel tar patienten läkemedlet, men inte enligt ordination. I mellan en tredjedel och en fjärdedel hämtas den förskrivna medicinen aldrig ut. - Jag tror att det till stor del är ett kommunikationsproblem mellan läjare och patient, säger Foldevi. Margareta Fallsberg undervi-sar i patientkommunikation och medicinsk följsamhet vid Linköpings universitet och har författat boken ”Tankar om mediciner och medicinering” som på djupet också analyserar pedago-giska problem kring medicinering. Aktuella forskningsresultat gäller inte specifikt diabetes utan mer allmänt.
Red
upp
Sildenafil reverses diabetic
gastroparesis in mice
Från J Clin Invest 2000;106:373-384.The phosphodiesterase inhibitor sildenafil augments nitric oxide signaling and reverses the symptoms of gastropathy in two murine models of diabetes, researchers report in the August issue of The Journal of Clinical Investigation. Dr. Christopher D. Ferris and colleagues from The Johns Hopkins University in Baltimore, Maryland, generated genetic and streptozotocin induced models of diabetes in mice. The mice exhibited defects in gastric emptying and nonadrenergic, noncholinergic relaxation of pyloric muscle similar to that of mice lacking the neuronal nitric oxide synthase gene (nNOS), the investigators report.
In addition, Dr. Ferris’ group observed a pronounced reduction in pyloric nNOS protein and mRNA in the mice. Insulin implants returned nNOS expression and pyloric function to normal levels. ”Thus, diabetic gastropathy in mice reflects an insulin sensitive reversible loss of nNOS,” Dr. Ferris and colleagues conclude. Further experiments revealed that delayed gastric emptying could also be reversed by administration of sildenafil, which ”augments NO signaling.” ”These findings have implications for novel therapeutic approaches and may clarify the etiology of diabetic gastropathy,” the authors say.
In an interview with Reuters Health, Dr. Ferris (soon to be at the Vanderbilt University Medical Center in Nashville, Tennessee) said that the use of sildenafil to treat gastroparesis ”may not be a long way off.” He added, ”We have clinical trial protocols written now,” and ”pilot trials could begin in September.”He noted that even though insulin also reverses gastroparesis in diabetic mice, a lot of insulin-treated diabetic patients still experience this condition and sildenafil has the potential to help these patients.
”Within a year,” he said, ”we expect to be able to determine if [sildenafil] is efficacious in humans.” The best known effect of sildenafil to treat erectile dysfunction probably will not be an issue for most patients.
”Sil-denafil allows people to have erections. It works only in the proper context, so we don’t expect that to be a problem,” Dr. Ferris commented.
upp
Det metabola syndromet är relaterat
till tjocka vänsterkammar-väggar men
inte till vänsterkammar-hypertrofi
Av Johan Sandström, Uppsala.Vänsterkammarhypertrofi, en av de viktigaste kardiovaskulära riskfaktorerna, är ett tillstånd med till stor del okänd etiologi. I en artikel den 6 juni i Circulation (1) belyses sambanden mellan vänsterkammarens geome-tri och faktorer i det metabola syndromet (obesitas, hypertoni, dyslipidemi, glukosintolerans och insulinresistens). Analyserna är utförda i en stor population 70- åriga män boende i Uppsala, undersökta med bland annat ekokardiografi, hyperinsulinemisk euglykemisk clamp, oralt glukos-toleranstest (OGTT) och 24- timmars ambulatorisk blodtrycks och pulsmätning. Relativ vänsterkammarvägg-tjocklek (väggtjocklek/inner-diameter) var signifikant relaterad till insulinkänslighetsindex, (r= -0.14), glukos- och insulinnivåer vid OGTT, 32-33 split-proinsulin, triglycerider, fria fettsyror, midja-/ stusskvot, body mass index, 24- timmarsblodtryck och puls (r=0.10-0.22). Endast systoliskt 24-timmarsblodtryck (r=0.15), puls (r= -0.14) och insulin efter 2 timmars OGTT (r= -0.10) var signifikant relaterade till vänsterkammarmasseindex (se figur).
Sammanfattningsvis var flera komponenter i det metabola syndromet relaterade till tjocka vänsterkammarväggar med normal innerdiameter (concentric remodeling), men inte till vänster-kammarhypertrofi, i denna populationsbaserade studie av äldre män.
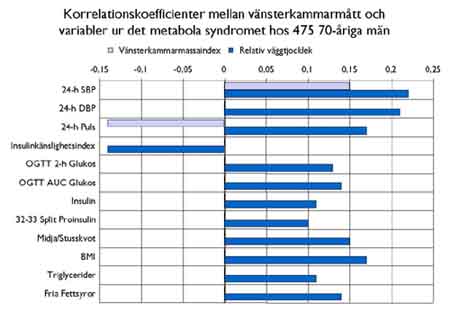
Dessa resultat överensstäm-mer med en tidigare populations-studie (2), men skiljer sig från ett flertal mindre studier med varierande inklusionskriterier och ofta bristande indexering av vänsterkammarmassa för kroppsstorlek. Vad gäller eventuella orsakssamband kan man spekulera i om den trofiska effekt av insulin på myocardiet som har visats i djurmodeller, hos människa inskränker sig till att påverka muskelfibrernas tjocklek och därmed vänsterkammarväggtjockleken, och inte vänster-kammarens innerdiameter.
Concentric remodeling har tidigare relaterats till en ökad perifer kärlresistens, vilket kan bero på minskad kapillarisering av bland annat skelettmuskulatur, vilket även observerats vid det metabola syndromet. Studien visar att män med det metabola syndromet i ökad utsträckning har förtjockade vänsterkammarväggar med normal innerdiameter (concentric remodeling), en vänsterkammar-geometri som är förknippad med en ökad kardiovaskulär risk. Denna hjärtgeometriförändring kan kanske vara ett patofysiologiskt steg i händelsekedjan mellan utvecklande av det metabola syndromet och senare kardiovaskulär sjuklighet och död.
Mer om vår kohort och publikationer kan läsas på www.pubcare.uu.se/ ULSAM/
Johan Sundström
Inst. f. Folkhälso- & Vårdvetenskap
Geriatrik, Uppsala Universitet
Box 609, 751 25 Uppsala
Fax 018-6117976
E-post: johasund@mail.anst.uu.se
upp
Referenser
1. Sundstrom J, Lind L, Nystrom N, Zethelius B, Andrén B, Hales CN, Lithell HO. Left Ventricular Concentric Remodeling Rather Than Left Ventricular Hypertrophy Is Related to the Insulin Resistance Syndrome in Elderly Men. Circulation 2000;101:2595-2600.
2. Ohya Y, Abe I, Fujii K, Ohmori S, Onaka U, Kobayashi K, et al. Hyperinsulinemia and left ventricular geometry in a work-site population in Japan. Hypertension 1996;27(3 Pt 2):729-34.Från Läkartidningen. Publikation
sker med tillåtelse från författaren och LT.Red