Referat
Introduktion
Metod
Resultat
Praktiskt tillämpning
Afternoon office visits may miss diabetes diagnosis
Kommentar
Sense of humor might be cardioprotective
Statins seem to work especially on vulnerable plaque
Fler och yngre barn insjuknar i diabetes
Glycemic control may improve left ventricular hypertrophy in diabetics
Big jump in diabetes linked to obesity
Fish oil lowers TG with little or no glycemic effect in type 2 diabetics
More studies needed to justify hyperbaric O2 for diabetic foot ulcers
Glucose-dependent insulin release achieved in non-beta cells
Metabolic syndrome components have independent effects on diabetes risk
Lower cut-off for fasting glucose identifies more patients at risk of diabetes
Beteende-förändring - Hur?
Forskare fann mekanismen bakom typ 2 diabetes
Economic impact of multiple insulin injection therapy for type 2 diabetic patients
Diabetespatientens bästa vän: en hund
Diabetes-related preventive-care practices deemed inadequate
Forskare identifierar mottaglighetsgener för diabetes
Framgångsrik genterapi mot typ 1 diabetes
Banbrytande
Problem tidigare
Goda resultat
Obesity linked with increases in type 2 diabetes and healthcare costs
NPH x 2 daily beats ultralente x 1 in type 2
Tight metabolic control in diabetic pregnancy necessary for normal fetal growth
Lipid-carbohydrate interactions inreduced muscle insulin sensitivity
Distal pancreatectomy increases risk for diabetes in pancreatitis patients
Blood glucose levels have prognostic value in acute pancreatitis
High TG in diabetic women threaten outcome of ACB
Diabetics on orlistat can lose less weight than nondiabetics to reduce CVD risk
Diabetes typ 1 och graviditet
Kort sammanfattning av en studie av Marie Berg och Marja-Liisa Honkasalo publicerad i Journal of Psychosomatic Obstetrics & Gynecology 2000 (21): 39-48.
Introduktion
Graviditet och moderskap är en viktig period då kvinnans fysiska och mentala välbefinnande är direkt kopplat till såväl den egna som barnets hälsa (1). Perioden har beskrivits både som en kris och som en övergång, ”transition”, från en livsfas till en annan (2-7). Kvinnor med insulin-behandlad diabetes utgör den enskilt största gruppen med kronisk sjukdom som genomgår graviditet och förlossning, med en prevalens på 0,2 - 0,4% i Europa. I Sverige låg siffran på 0, 33% år 1997 (8,9). Chansen för en kvinna med diabetes typ 1 att föda ett friskt barn har ökat avsevärt alltsedan insulinbehandling blev möjlig, men särskilda framsteg har gjorts under de senaste årtiondena (10). Genom framför allt god blodsockerbalans och noggrann vård initierad redan före befruktningen har såväl obstetriska som neonatala risker minskat.
Fortfarande betraktas dock graviditet och förlossning som en medicinsk högrisk med såväl ökad missbildningsfrekvens som ökad perinatal morbiditet och mortalitet. Graviditetskomplikationer som havandeskapsförgiftning och intrauterin tillväxthämning och tekniska interventioner som kejsarsnitt är mer frekventa (11-15). God glykemisk balans erhålls genom täta blodsockermätningar, intensifierad insulinbehandling samt regelbunden måltidsordning och livsstil. Detta medför ökad frekvens av hypoglykemiattacker liksom en ökad stressnivå (18). Det är viktigt att få ökad kunskap om upplevelser i samband med övergång i moderskapet. Syftet med studien var att beskriva hur kvinnor med insulinbehandlad diabetes upplever sin livssituation under graviditeten.
till toppenMetod
En kvalitativ metod med hermeneutisk fenomenologisk ansats enligt Van Manen användes (19). Syftet med denna metod, som grundar sig på de fenomenologiska och hermeneutiska filosofierna (20,21), är att fånga och beskriva den essentiella strukturen i en livsupplevelse. Urvalet utgjordes av 14 kvinnor som var inskrivna vid Antenatalenheten, Sahlgrenska universitetssjukhuset.
Åtta väntade första barnet och sex var omföderskor. Åldern varierade mellan 25-38 år med en medianålder på 28 år. Sju av kvinnorna hade haft diabetes mer än 10 år, sju mer än 20 årvarav tre med avancerade kärl-komplikationer. Kvinnorna intervjuades tre gånger under graviditeten; graviditetsvecka 11-15, graviditetsvecka 22-27 och graviditetsvecka 32-39. Totalt genomfördes 44 intervjuer på 45-120 minuter som spelades in på band. Intervjuerna hade en öppen och följsam karaktär med en initial fråga: kan Du beskriva hur Du upplever Din graviditet? Intervjuerna skrevs ner ordagrant, hela materialet genomlästes åtskilliga gånger med beaktande av såväl helhet som variationer. Utifrån meningsbärande uttryck utvecklades slutligen en essentiell struktur19.
till toppenResultat
Alla kvinnor förbättrade sina blodsockernivåer. Medel-HbA1C för gruppen ändrades från 7,1 % i början av graviditeten, till 5,4 % strax före förlossningen. Kvinnorna mätte ofta blodsockervärdet mer än 10 gånger per dygn.
Den essentiella strukturen av upplevelsen av att vara gravid för kvinnor med insulinkrävande diabetes kan sammanfattas ” barnet kräver det” och innefattar två teman 1) objektifiering och 2) ett extremt ansvarstagande. I respektive tema finns olika delar vilka är sammanfattade i figur 1. Alltifrån konstaterad
graviditet sattes barnet först.I objektifieringen uttrycks kvinnornas insikt om att deras graviditet klassades som en risk med en ökad medvetenhet om att deras kropp inte var normal. De upplevde det lite som att få diabetes på nytt och för många aktiverades den inte färdigbearbetade sorgen över att vara sjuk. Hotet om att någon komplikation skulle inträffa någon gång under graviditeten låg över dem.
De kände inte igen sin kropps signaler och de täta blodsocker-provtagningarna gav en insikt om att känslan inte alltid stämde med det uppmätta värdet. De upplevde en förlust av kontroll där blodsockret i stället kom att styra hela livssituationen. Detta medförde ett ökat beroende av framför allt sjukvård-sexpertisen men också av anhöriga. På samma gång utvecklade kvinnorna ett ökat ansvarstagande för barnet, innefattande en ständig oro, en ständig press med känsla av otillräcklighet samt en ständig självförebråelse.
till toppenPraktiskt tillämpning
Obstetriker, barnmorskor, diabetologer, diabetessjuksköterskor och andra aktuella vårdgivare har en viktig uppgift i att stödja dessa kvinnor under graviditeten så att oron, pressen och självförebråelsen kan minska. Genom att hjälpa gravida kvinnor med diabetes att få en ökad tilltro till sig själva kan de stärkas i sin modersidentitet. Att göra detta samtidigt som vikten att följa en strikt noggrann livsstil betonas, är en utmaning för varje vårdgivare som möter dessa kvinnor.Vill Du veta mer?
Kontakta Marie Berg, Antenatal-enheten
SU/Östra, Göteborg.
Telefon 031-3436661
E-post: marie.a.berg@vgregion.se
Referenser kan fås från författaren.
till toppenAfternoon office visits
may miss diabetes diagnosis
Från JAMA 2000;284:3157-3159.
Application of current diabetes diagnostic criteria to patients seen during afternoon office visits may miss half of the patients who have undiagnosed diabetes, according to a report published in the December 27th issue of The Journal of the American Medical Association. This occurs as a result of the diurnal variation in fasting glucose, where levels are higher in the morning than in the afternoon.
Dr. Maureen I. Harris, from the National Institute of Diabetes and Digestive and Kidney Diseases, in Bethesda, Maryland, and colleagues randomized 12,882 subjects, age 20 years or older, with no previously diagnosed diabetes to undergo a morning or afternoon fasting glucose evaluation.Fasting plasma glucose levels from morning-examined subjects were significantly higher than levels from afternoon-examined subjects, the authors note. As a result, only half as many afternoon-examined subjects had glucose levels greater than 126 mg/dL compared with morning-examined subjects.
The fasting glucose level diagnostic of diabetes would have to be reduced to 114 mg/dL or greater in afternoon-examined patients, Dr. Harris’ team calculated, in order to achieve a prevalence comparable to that in morning-examined subjects when the standard level of 126 mg/dL or greater was employed.”Many patients in the ambulatory care setting are seen in the afternoon, and these patients can be asked to fast for at least 4 hours before testing for diabetes,” the researchers point out. ”Regardless of the time of day that patients are tested, physicians need to confirm the diagnosis by repeat testing on a different day.” ”Early morning rises in fasting glucose levels and insulin requirements (the ’dawn phenomenon’) have been observed in patients with diabetes and in some, but not all, studies of nondiabetic persons,” the authors note. ”Our data showing higher fasting levels of plasma glucose, serum insulin, and serum C peptide in morning subjects are consistent with the existence of a dawn phenomenon in nondiabetic subjects.”
Red
till toppenKommentar
Det var en intressant artikel. Den visar ju övertygande att det finns en diurnal variation i glukosvärdena, och drar kliniska konsekvenser av det. Om man därför vill använda eftermiddagsvärdena i diagnostiken måste man ha speciella referensvärden för dem, det räcker inte att ha samma kriterier som i fastande morgonvärde. Detta, menar jag, är ytterligare en kritisk synpunkt på ADA-kriterierna, och kan sägas ytterligare markera att vi bör arbeta vidare på kriterierna. Man kan också hävda att om OGTT används undanröjer man en del av dessa svårigheter, även om det i nuläget inte finns tillräckligt med dataunderlag rörande gränser vid användandet av OGTT på eftermiddagen.Bo Ahrén, professor Department of Medicine Lund
University, Fax +46 222 0757
E-post: Bo.Ahren@med.lu.se
Sense of humor might
be cardioprotective
Från American Heart
Association Meeting, USA, New Orleans november 2000.
Patients with coronary heart disease fail to find much humor in life, Baltimore researchers report. On the other hand, patients with a high ”humor score” have a reduced risk of CHD. Since anger and hostility have been linked to CHD, Dr. Michael Miller and colleagues from the University of Maryland wondered if the converse were true—if those who tend to find humor in life have healthier hearts.
The investigators chose a group of 150 patients who had had either myocardial infarction or bypass surgery and measured their sense of humor against 150 controls, frequently the spouses or relatives of the patients. ”We purposely stayed away from patients in acute MI,” Dr. Miller said, so that the actual episode of ill health would not be a factor in the responses.Both groups answered two questionnaires, one designed to assess how much humor they found in a series of 20 hypothetical situations, and the other a standard tool designed to assess anger and hostility.
”Patients with heart disease had a 40% to 45% decreased likelihood of responding with laughter” to the situations in the first questionnaire, Dr. Miller reported. Meanwhile, ”those who responded with laughter had the lowest likelihood of anger and hostility,” Dr. Miller said. ”There was an inverse relationship.” In addition, patients who showed a high tendency to laugh had a significantly reduced risk of CHD after the researchers controlled for age and sex.
Because anger and hostility are known to constrict the blood vessels, Dr. Miller and colleagues will now measure a vasodilator to determine if it is released during laughter. ”We’re going to measure nitric oxide,” Dr. Miller told Reuters Health. ”It’s in the same family as laughing gas.” Dr. Miller thinks that laughter should be incorporated into every cardiac rehabilitation program, to be used as a form of exercise. ”Much of our behavior is learned behavior,” he said, ”and we can learn to regulate the laughing muscles.”Red
till toppenStatins seem to work especially
on vulnerable plaque
Från American Heart Association Meeting, USA, New Orleans november 2000.
For the first time inhumans, reserachers have used magnetic resonance imaging (MRI) to show that a cholesterol lowering drug removes the fat build-up from atherosclerotic lesions, stabilizing the plaque that is most likely to cause a heart attack or a stroke.
- This is the first study which, by direct visualization, shows that cholesterol lowering by statin drugs reduce the amount of lipids deposited in artery walls”, says lead author Robert Corti at the Cardiovascular Biology Research Laboratory at Mount Sinai Hospital in New York. Statin drugs, like the simvastatin that was used in this study, are very effective at lowering blood cholesterol. High cholesterol levels are associated with plaque buildup on arterywalls and an increased risk of heart disease. In large clinical trials, statins have been associated with 30-35% reductions in heart attacks, unstable angina and strokes - for diabetics 55% risk reduction.
However, their mode of action has been unclear. One hypothesis is that statins may reduce the fat content of plaque, making them more stable. Until now, this hypothesis could not be tested by conventional imaging techniques, such angiography, which does not show the artery wall, notes Corti. Refinements in MRI technique now allow visualization of the artery wall as well as the artery cavity.
- The painless, non-invasive procedure could someday making imaging the artery as easy and routine as getting a mammogram. The Mount Sinai group has identified important details about athersosclerotic plaque including finding that all plaques are not critical: cholesterol-rich plaques are the most likely to rupture and cause heart attacks and strokes. Plaques does not cause problems as long as it stays in the artery wall. When plaque ruptures, the body tries to rupture the damage by forming blood clots, which can cause heart attacks or strokes by blocking the blood vessels, reserachers say. Vulnerable plaques with its core contain lipids and scavenger cells as macrophages that damage the vessel wall. It has a large amount of chemical that stimulates the formation of blood clots.In the study 50 patients were enrolled during 12 months with total cholesterol between 200-240 mg/dl and atherosclerotic lesions. They were randomly assigned to receive daily simvastatin doses of either 20 or 80 mg. The research-ers imaged more than 600 segments of the subjects´ aortas and carotis arteries at baseline and after 6 and 12 months of treatment of simvastatin. Significant reductions in LDL-cholesterol was seen after 6 weeks in the simvastatin groups. It took 12 months for changes to appear in the artery wall.
- Although the diameter of the artery cavity did not change, the vessel wall area shrank by 8-10%, indicating that the plaque has regressed, Corti reports. These are not people with heart attacks ansd they do not have particularly high blood cholesterol. They are the kind of people the doctors see and have to make decisions about each day. By this MRI technique makes it possible to someday detect blood vessel disease much earlier in the disease process, before a patient shows symtoms or signs of disease.
# Abstract 2234, American Heart Assocation, New Orleans, USA, Circulation Nov 2000 Suppl.Red
till toppenFler och yngre barn insjuknar
i diabetes
Från Acta Paediatrica 2000;89:1231-1237.
Insjuknandefrekvensen per år i diabetes under barn- eller ungdomstiden ökar hastigt i Sverige och trenden pekar mot lägre åldrar. Gisela Dahlquist, professor på Barnkliniken vid Norrlands Universitetssjukhus, och L Mustonen vid Epidemiologen, Umeå Universitet, har analyserat de 8.358 individer som insjuknat i diabetes före vuxen ålder i Sverige under perioden 1978 till 1997. Under 1978 debuterade drygt 24 barn per 100.000 i diabetes, mot knappt 32 per 100.000 barn under 1997.Andelen barn som fick diabetes ökade därmed med 1.7 procent per år. Under de första tio åren ökade insjuknandet flest i åldrarna fem till 9 år. De sista tio åren låg den största ökningen hos de ännu yngre.
Som utlösande faktorer hos individer med disposition för sjukdomen har tidigare noterats vissa virusepidemier. Undersökningen bekräftar detta, om än svagt. Man fann ingen relation förändringar i vaccinations- eller amningsmönstret i landet. Man vet dock att tidig diabetes är relaterat till snabb tillväxt, som i sin tur är korrelerat till stigande allmänt välstånd.Red
till toppenGlycemic control may improve left ventricular
hypertrophy in diabetics
Från Am J Hypertens 2000;13:1149-1154.
In hypertensive patients with type 2 diabetes, better control of blood glucose may contribute to a regression in left ventricular hypertrophy (LVH), according to a report by Brazilian researchers. Dr. Maria Teresa Zanella, from Hospital do Rim e Hipertensao, Sao Paulo, and colleagues studied 56 hypertensive men and women with type 2 diabetes, along with 26 healthy controls. The researchers obtained echocardiograms and calculated mean blood pressure, fasting blood glucose levels, cholesterol and fractions, and triglyceride levels, for 4 years before the study period.At baseline, the researchers found that compared with nondiabetic hypertensive controls, patients with type 2 diabetes had an increased left ventricular mass index and abnormalities in diastolic function. The team then followed the diabetic patients for 1 year, during which time these patients had blood pressure, fasting blood glucose, and lipids measured every 2 months. After the year, patients once again underwent echocardiography, according to their report in the November issue of the American Journal of Hypertension.
On follow-up, Dr. Zanella’s group noted that 22 patients had a greater than 10% reduction in left ventricular mass index, while 17 patients had a greater than 10% increase. There was no change in left ventricular mass index in the 17 remaining patients. The investigators report that the only factor independently associated with a reduction in left ventricular mass index in the 22 patients was a reduction in blood glucose, from 178 mg/dL to 147 mg/dL. They also found a correlation between blood glucose and left ventricular mass index percent variations. Dr. Zanella’s group found no significant changes in diastolic function, after 1 year for any of the patients.Red
till toppenBig jump in diabetes
linked to obesity
-76% rise of diabetes in age 30-40 years.
From Diabetes Care 2000;23:1278-83 and The Lancet 2000;356;834.
The prevalence of diabetes in the USA has jumped 33% in the past decade - a rise that seems to be linked to the growing number of Americans who are obese, a new study reports in Diabetes care 2000;23:1278-83. The increases were seen in both sexes, in all age groups, all ethnic groups, and at all education levels. ”It was across the board”, says study author Michael Engelau of the USCenters for Disease Control (CDC) and Prevention.Most worrying, he adds, is the 76% rise in diabetes among men and women in their 30s. Engelau and hos co-workers used data collected from an ongoing project being done by the CDC and 43 states. The researchers compared the results of telephone surveys done in 1990-98. People were asked their weight and whether their doctor had told dem that they were diabetic. Prevalence of diabetes has risen from 4.9% in 1990 to 6.5% in 1998, which puts the number of people with diabetes today at 13 million. The findings suggest that diabetes care is going to become a growing burden for the US health care system.
9% risk for diabetes per added kg Much of the blame for the problems seems to lie with the rapid rise in obesity, Engelau says.”Obesity is tracking in parallel to the rise in diabetes.” The study found, for example that an average for every added kg in wight, a person´s risk of diabetes rose by about 9%.
Such a risk may indicate that many are already dangerously overweight, making even a small gain enought to push them over the diabetic threshold, Engelau says. And it is likely that the upsurge in obesity is going to continue to drive up the prevalence of diabetes, he warns.Red
till toppenFish oil lowers TG with little or no glycemic
effect in type 2 diabetics
Från Diabetes Care 2000;23:1407-1415.
The results of a metaanalysis of 18 trials conducted over a 10-year period show that fish oil supplementation for patients with type 2 diabetes lowers triglycerides but has no statistically significant effect on glycemic control. ”This study disproves the long-held belief that fish oil supplementation adversely affects glycemic control in patients with type 2 diabetes,” Dr. Victor M. Montori told Reuters Health. Dr. Montori, of the Mayo Clinic and Foundation, Rochester, Minnesota, and colleagues collected data on glycemic control and lipid levels in 823 patients with type 2 diabetes who took fish oil supplements in daily dosages ranging from 3 g to 18 g.Most patients, who were followed for a mean of 12 weeks, were men between 55 and 65 years of age who had had type 2 diabetes for between 5 and 10 years. In the September issue of Diabetes Care, the researchers write that ”fish oil supplementation did not result in any statistically or clinically significant increase in fasting glucose or glycosylated hemoglobin.”
The main effect of fish oil supplementation was ”the reduction of triglycerides by an average of 0.56 mmol/L,” Dr. Montori told Reuters Health. Conversely, he reported a ”small increase [0.21 mmol/L on average] in low-density lipoprotein cholesterol.”
The increases in LDL cholesterol and reductions in triglycerides were ”most marked in those trials that recruited hypertriglyceridemic subjects and used higher doses of fish oil,” the researchers write. Theynote that triglycerides levels were reduced up to 4 mmol/L in patients with hypertriglyceridemia. While the pooled data ”was not able to elucidate the ideal dose of fish oil needed to achieve large reductions in triglycerides,” Dr. Montori said, it suggests that ”fish oil may be safe to add to the armamentarium of triglyceride-lowering medication” for people with diabetes.Red
More studies needed to justify
hyperbaric O2 for diabetic foot ulcers
Från Diabetes Care 2000;23:1551-1555.In a review of medical
literature, researchers identified only seven studies involving systemic hyperbaric oxygen therapy for diabetes-related foot pathology, Dr. Robert P. Wunderlich reports. While the existing literature is promising, ”additional randomized controlled studies in large diabetic populations would further lend credence to the common assumption that hyperbaric oxygen therapy is a beneficial adjunctive treatment for diabetic foot wounds,” Dr. Wunderlich, of the Diabetex Foot Care Center in San Antonio, Texas, told Reuters Health. In the October issue of Diabetes Care, Dr. Wunderlich and colleagues report that of the 76 studies his group identified through MEDLINE, 21 involved humans.Seven studies involved diabetic foot pathology and ”only five were designed as controlled studies that included a group that did receive hyperbaric oxygen therapy.” Furthermore, only two of the five controlled studies were randomized, Dr. Wunderlich said.
In the controlled studies 28 patients, on average, received hyperbaric oxygen therapy, compared with 16.2 controls. The most recent and, according to Dr. Wunderlich, the most convincing study demonstrated fewer above- or below-the-knee amputations among patients with Wagner grade IV foot wounds compared with controls. ”However, the study also showed that there was no difference in minor amputations for any grade of wound, and no difference in major amputations for Wagner grade I to grade III wounds,” he told Reuters Health.The results of this study suggest, he said, that ”only patients with gangrene of the forefoot could expect fewer major amputations when adjunctive hyperbaric oxygen therapy is incorporated into their treatment plan.” Dr. Wunderlich and his colleagues conclude in the journal that ”given the substantial cost associated with these treatments, a more thorough analysis of human studies dealing with hyperbaric oxygen therapy for the diabetic foot is not only justified but necessary.”
Red
till toppenGlucose-dependent insulin release
achieved in non-beta cells
Från Science 2000;290:1959-1962.Gut K cells can be genetically engineered to release insulin in response to glucose levels, according to a report published in the December 8th issue of Science. ”Many groups have been striving to recreate physiological insulin production from ’surrogate’ cells. However, it turns out that the beta cells are very specialized and difficult to duplicate,” Dr. Timothy Kieffer from the University of Alberta in Edmonton, Canada, told Reuters Health. ”We targeted naturally existing meal-responsive endocrine cells for insulin replacement.”
Dr. Kieffer and colleagues experimented with a line of gut K cells, which normally secrete the insulin potentiating hormone GIP in response to a meal. They transfected the cells with a construct of the human preproinsulin gene linked to the GIP regulatory region, and found that the transfected cells not only secreted human insulin and C peptide in correct proportions, but also did so in a glucose-dependent fashion.
Moreover, transgenic mice generated by injecting the GIP/ insulin construct into embryonic pronuclei expressed human insulin in the duodenum and stomach but not elsewhere, the authors report. Histological studies confirmed that human insulin production was restricted to gut K cells. These transgenic mice produced human insulin in response to an oral glucose challenge, the report indicates. Furthermore, when beta cells where destroyed in the animals they exhibited neither fasting hyperglycemia nor glucosuria. ”Our findings suggest that insulin production from gut K cells may correct diabetes to the extent of restoring normal glucose tolerance,” the authors conclude. ”Genetic engineering of gut K cells to secrete insulin may represent a viable mode of therapy for diabetes, freeing patients from repeated insulin injections and reducing or even eliminating the associated debilitating complications.”
”It is important to note that this is a basic research proof-of-concept study which, in its present stage, cannot be applied to patients,” Dr. Kieffer cautioned. ”Nevertheless, this and other recent studies show that insulin replacement by gene therapy may eventually be feasible for patients with diabetes.”Red
till toppenMetabolic syndrome components have
independent effects on diabetes risk
Från Diabetes Care 2000;23:1242-1248.The individual components of the metabolic syndrome have independent effects on the 5-year risk of developing impaired glucose tolerance (IGT) or diabetes, according to researchers in Finland, the US and the UK. The fact that these effects are not synergistic ”raises the possibility that multiple mechanisms may lead to [glucose intolerance],” Dr. Edward J. Boyko, of the Veterans Affairs Medical Center in Seattle, Washington, and colleagues say in the September issue of Diabetes Care.
Dr. Boyko and his team examined the contributions of individual components of the metabolic syndrome to the risk of developing IGT and diabetes in a cohort of 2605 adult residents of Mauritius, an island in the south-western Indian Ocean. All of the patients were normoglycemic at the start of the study. During 5 years of follow-up, 2.9% of patients developed IGT and 1.3% developed diabetes.”All features of the metabolic syndrome that we considered were related in the univariate analysis to a higher risk of worsening of glucose tolerance among members of this multiethnic study population,” the investigators write.
But after they controlled for several demographic and family history characteristics that could affect the risk of IGT or diabetes, only five components of themetabolic syndrome significantly and independently predicted these two outcomes: fasting glucose, 2-hour glucose, waist-to-hip ratio, body mass index and serum uric acid.
”This result should not be interpreted as refuting a role for insulin resistance in the pathogenesis of diabetes because glucose level in the fasting and stimulated states is in part a function of insulin sensitivity,” Dr. Boyko and colleagues note. Two additional metabolic syndrome components, serum triglyceride and plasma leptin, were significantly but nonlinearly associated with the development of IGT or diabetes. ”At higher concentrations of triglycerides and leptin, risk plateaus and even declines slightly,” the authors explain. Both associations were ”unexpected,” they add, and ”will require further investigation.”Red
till toppenLower cut-off for fasting glucose
identifies more patients at risk of
diabetes
Från J Clin Endocrinol Metab 2000;85:3101-3108.Lowering the currently recommended fasting glucose cut-off to 5.72 mmol/L helps identify a larger number of patients at risk of diabetes, and could help reduce the previously reported discordance between the American Diabetes Association (ADA) and World Health Organization (WHO) criteria for the diagnosis of diabetes.Because of their different requirements for diagnosing diabetes, the ADA criteria for fasting glucose testing are less sensitive than the glucose tolerance testing criteria proposed by the WHO, according to an August 1999 Reuters Health report. In the September issue of The Journal of Clinical Endocrinology and Metabolism, Dr. Arnold von Eckardstein and colleagues, from Universitat Munster, in Germany, propose a refinement to both sets of criteria that may help alleviate some of this controversy.
The team looked at the association between fasting serum glucose and the 6-year risk of developing diabetes in a cohort of 3737 men, aged 36 to 60, who were enrolled in the PROCAM (Prospective Cardiovascular Munster) Study. During the study, 200 of the men developed diabetes.
Fasting glucose was a stronger predictor of diabetes risk than global risk estimation using multiple risk factors. ”A glucose level of 5.72 mmol/L was the best discriminatory cut-off,” the investigators write, with a sensitiv-ity and specificity of 75.0% and 72.7%, respectively. This cut-off is lower and more sensitive and specific than the currently recommended cut-offs for fasting serum glucose.
On the other hand, individual risk factors for diabetes, such as age, blood pressure, cholesterol, family history and body-mass index, independently helped identify patients in a prediabetic state. When considered with other independent risk factors, the researchers conclude that fasting glucose can ”help to identify individuals who are at high risk for diabetes mellitus.”Red
till toppenBeteende-förändring
- Hur?
Det är tänkvärt att den som arbetar kanske mest intensivt med patienternas beteende, vars hela konsulttid går till att kartlägga och lösa beteendestörningar, nämligen dietisten - inte heller har tillräcklig utbildning i beteendevetenskapen. Se nedan abstract. Åtgärder behövs! Journal of Human Nutrition & Dietetics 13 (4) 287-298. Do dietitians feel that they have had adequate training in behaviour change methods? Av L. Rapoport & K. Nicholson Perry.
Aim: To investigate dietitians’ perceived adequacy of pre- and postregistration training in a range of behaviour change techniques, current main approach to dietary treatment and perceived usefulness of future training in five core behaviour change modalities.Method: A questionnaire was designed and distributed to all dietitians registered in the BDA membership base (n = 4202).
Results: Three hundred and ninety-four questionnaires were returned. The majority of these respondents had obtained their degree since 1982 (77%), since when courses were more likely to have contained a psychological component. Despite the fact that facilitating dietary behaviour change is a key dietetic role, respondents felt that they had not received adequate training in behaviour change skills in their dietetic training.Training was perceived to be most satisfactory in active listening skills, but this was perceived as barely adequate. Training was perceived as particularly poor in: applying theories of cognitive and behavioural therapy (CBT); motivational techniques; group work skills; and in both theory and skills of relapse prevention. Although 40% of respondents reported receiving explicitly psychologically based training, skills-based training (mainly counselling) was reported by only 25% and was limited by being mainly short 1- or 2-day courses.
Overall, where further training was obtained it was perceived to be more adequate than that reported within preregistration dietetic training.
Conclusion: Respondents felt that they had not received adequate training in behaviour change skills in their dietetic training.The application of CBT, motivational techniques and relapse prevention was perceived as particularly deficient in training and the majority of respondents felt that future training would be useful or very useful. In the current health service climate, where evidence based practice is crucial for all practitioners with the emphasis on improved quality of care with measurable outcomes, research must be funded and undertaken to support attempts to improve dietitians’ effectiveness as behaviour change agents
Mette Axelsen, klinisk näringsfysiolog
Red Dietistforum
E-post: mette.axelsen@medic.gu.seForskare fann mekanismen
bakom typ 2 diabetes
Från Nature Genetics november 2000 och Margareta William-Olsson GP 8/11 2000.Svenska forskare har gjort en upptäckt som innebär ett stort framsteg för förståelsen av typ 2 diabetes. Kraftverken i de insulin-producerande betacellerna fungerar inte. Denna mitokondriedefekt är en viktig orsak till att insulin inte frisätts som det skall, skriver GöteborgsPosten.
Det är docent Nils Gäran Larsson och proferssor Per Olof Berggren och deras forskargrupper vid Karolinska Sjukhuset som tillsammans med Anders Oldfors på Sahlgrenska lyckats påvisa denna funktionsnedsättning.Genom att använda en unik musmodell har forskarna lyckats att undersöka hur betacellernas kraftverk fungerar vid diabetes. De har visat att en nedsatt funktion hos mitokondirerna i betacellerna leder till en störning i cellernas signalsystem med nedsatt fri-sättning av insulin som följd och därmed diabetes. Är mitokondriefunktionen nedsatt en längre tid resulterar det i att de insulinproducerande betacellerna dör. Funktionen hos kraftverken är alltså grundläggande inte bara för betacellernas signaler och frisättning av insulin utan också för deras livslängd.
- Man har länge misstänkt att funktionen hos mitokondrien spelar en roll vid typ 2 diabetes. Nu har man kunnat visa det, säger Nils Göran Larsson. Det är en viktig kunskap för att i framtiden kunna rätta till fel i frisättningen av isnulin som föreligger vid diabetes. Andra forskargrupper har visat att mellan 1-2 procent av alla med diabetes har genetiska sjukdomar som påverkar direkt mitokondriefunkitoionen. De svenska forskarnas upptäckt presenteras i novembernumret av den ansedda tidskriften Nature Genetics.Red
till toppenEconomic impact of multiple insulin injection therapy for type 2 diabetic patients
Från The Kumamoto Group, IDF 2000 Mexico City (Abstract#522 i Diabetic Research and Clinical Practice, vol 50, suppl 1 S1-S474).To evaluate the cost and effectiveness of intensive insulin therapy for type 2 diabetic patients on the prevention of diabetic complications in Japan, we performed economic evaluation based on a randomized controlled trial. A total of 110 patients with type 2 were randomized into two groups, a multiple injection insulin therapy (MIT) group, or a conventional insulin injectiontherapy (CIT), and were followed up for 10 years. Economic evaluation was applied to evaluate both health and economic outcomes. As outcome measures for effectiveness of intensive insulin, the frequency of complications, such as neuropathy, nephropathy, retinopathy, macrovascular events, and diabetes-related death, was used.
Direct medical costs associated with diabetes care during 10 years were calculated and evaluated.
MIT reduced the relative risk in the progression of retinopathy by 67%, photocoagulation by 77%, pro-gression of nephropathy by 66%, albuminuria by 100%, and clinical neuropathy by 64%, relative to CIT. Moreover, MIT prolonged the period in which the patients were free of complication 2.0 years for progression of retinopathy, 0.3 years for photocoagulation, 1.5 years for progression of nephropathy, and 2.2 years for clinical neuropathy. The total cost per patient during 10-year period for each group was US dollar 30 310 and 31 525, respectively. The reduction of total costs in MIT over CIT was mainly due to reduced costs for management of diabetic complications. Our results showed that MIT was more beneficial than CIT in both cost and effectiveness. In conclusion, MIT is recommended for the treatment of type 2 diabetic patients who require insulin therapy a early as possible fro the perspective of both patients and health policy.Red
till toppenDiabetespatientens bästa vän:
en hund
Från Expressen 29/12 2000 och BMJ 2000;321:1565-1566.Non-invasive detection of hypoglycaemia using a novel, fully biocompatible and patient friendly alarm system by Mimi Chen, Mark Daly, Natt Williams, Susie Williams, Candy Williams and Gareth Williams. Räddningen för människor som lider av diabetes kan vara - att skaffa en hund, skriver Expressen.
Var tredje hund som lever med en diabetiker känner när deras husse eller matte får låga blodsockervärden och gör då allt för att varna dem.
Det låter otroligt, och forskarna kan inte förklara hur det går till. Men det är sant. I British Medical Journal diskuteras ingående fenomenet. Ovanligt nog är hundarna nämnda som medförfattare. De skriver att var tredje hund som lever med en diabetiker ändrar sitt beteende drastiskt när deras hussar eller mattar får känning av hypoglykemi, dvs lågt blodsocker. Oftast känner hundarna dessutom av problemen långt innan deras ägare känner någonting alls. Rapporten återges i brittiska tidningen the Times, och ingående beskrivs hur hundarna reagerar;• Hunden Natt, 3 år, kan till och med känna av hur blodsockret sjunker hos sin matte genom sovrumsdörren när hon ligger och sover. Då skäller han och skrapar med tassen på sovrumsdörren tills hon vaknar
• Tiken Susie, 7 år, väcker henne när blodsockret har sjunkit och vägrar sedan somna om innan matte mår bra igen. Forskarna var mycket imponerade av dessa hundar som väcker sin ägare även då de sover. Något som ingen glukosmätare klarar av.Hur hundarna bär sig åt vet forskarna inte. En möjlig teknik skulle kunna vara en ändring i hundägarnas lukt som hundarna kan känna av. En annan är att de märker på husse och matte att de inte reagerar på deras signaler som de brukar.
-Vi tilltalas av föreställningen om det så kallade sjätte sinnet som hundarna brukar sägas ha. Men är väl medvetna om att något sådant först måste bekräftas genom ytterligare forskning, skriver läkarna i BMJ-artikeln. Forskarna hoppas att de ska kunna ta reda på vad som får hundarna att reagera somde gör, så att man därefter kan lära andra hundar att hjälpa sina ägare på samma sätt.Red
Diabetes-related preventive-care
practices deemed inadequate
Från Mortality and Morbidity Weekly Report 2000;49:954-958.ATLANTA (Reuters Health)- Current levels of preventive care for diabetic patients fall far short of Healthy People 2010 goals, the Centers for Disease Control and Prevention (CDC) concludes in the October 27th issue of the Mortality and Morbidity Weekly Report.
Researchers analyzed data from the 1997 to 1999 Behavioral Risk Factor Surveillance System (BRFSS), a random-digit-dialed telephone survey of the civilian non-institutionalized US population over age 18 years.Respondents with diabetes were asked questions about four preventive care practices: annual dilated eye examination, annual foot examination, selfmonitoring of blood glucose, and glycosylated hemoglobin (HbA1C) measurement. ”This report summarizes the results of that analysis, which indicate that levels of preventivecare practices among persons with diabetes are lower than the national health objectives for 2010,” the authors of the report note. The levels of preventive care for each practice varied by state and by demographic group, but overall were some 15% to 20% lower than the goals.
”One of the things that we are trying to do with this report is to establish a baseline for the 2010 objective of where we would like states to be,” Edward Tierney, an epidemiologist with the CDC’s National Center for Chronic Disease Prevention and Health I samarbete med Craig Hanis vid the Human Genetics Center,the University of Texas, Houston, Promotion, told Reuters Health.
”It is something that is going to involve a collaborative effort of the healthcare systems, healthcare providers, public health officials and patients,” said Tierney, who added, ”There is sometimes an impression that you can’t do anything about diabetes, and the message that we are trying to get out is that you can do something about it.”Red
till toppenForskare identifierar
mottaglighetsgener för diabetes
Från Nature Genetics och University of Chicago,Graeme Bell och medarbetare vid the Howard Hughes Medical Institute, University of Chicago, har identifierat ett antal gener som ökar mottagligheten för diabetes. Typ 2 diabetes innebär att kroppen inte kan tillverka sitt eget insulin eller att den inte kan använda sitt insulin på ett effektivt sätt. Obehandlad ansamlas socker i blod vilket kan leda till komplikationer i hjärta/kärl, njurar, ögon och nerver.
Diabetes är en mycket komplex sjukdom som orsakas av ett antal gener som verkar tillsammans med miljöfaktorer som fetma och saknad av motion/träning.Detta har medfört svårigheter för forskarna. En annan svårighet är att sjukdomen ofta inträffar efter 40 årsåldern vilket har gjort det svårt att samla ihop familjer med diabetes i släkten eftersom man då måste samla ihop drabbade över ett antal generationer. I samarbete med Craig Hanis vid the Human Genetics Center,the University of Texas, Houston, samlade forskarna data från 350 bröder och systrar med diabetes i en församling av mexikan- amerikaner, en etnisk grupp som har hög förekomst av diabetes (10.6%) På grundval av tidigare studier kunde forskarna identifiera att en tidigare okänd gen på kromosom 2 kodar för ett protein, calpain 10.
Calpainer är sk proteaser, proteiner som reglerar andra proteiners funktioner dvs gör dem mer eller mindre aktiva genom att klippa bort delar av proteinerna. De finns i alla celler hos alla djur. Just calpain 10 genen innehåller 15 funktionella enheter. Genom klippning och klistring av dessa enheter tillverkar kroppen åtta olika versioner av genen. En version av genen återfinns bara hos de insulinproducerande cellerna i bukspottskörteln.
Bells forskargrupp fann att sjukdomsrelaterad förändring återfanns i en del av calpain 10 genen (intron)som separerar de funktionella enheterna (exon). Delen ingår i de DNA delar som allmänt kallas "skräp DNA" eftersom det inte tros ha någon aktiv funktion i genen.
Denna genetiska förändring (mutation) agerar på ett recessivt sätt dvs endast individer som ärver två kopior av den muterade genen har ökad risk för diabetes. Mottaglighet för diabetes är än mer komplex eftersom forskarna även fann två andra genetiska variationer inom genen som bidrar till diabetes. Alla tre identifierade mutationer arbetar i samspråk för att ge ökad risk för diabetes hos affekterade personer.
Förståelse av mekanismen bakom de identifierade mutationerna kan leda till nya läkemedel mot diabetes, skriver Bell. Förhoppningen är att de genetiska studierna skall kunna hjälpa läkare att identifiera vilka yngre personer som är mottagliga för diabetes och intervenera med adekvat kost och träning i ett tidigt stadium.Referens: Nature Genetics samt University of Chicago.
Onlineadress: www.uchospitals.edu/ news/niddm1.htmlRed
till toppenFramgångsrik genterapi mot typ 1 diabetes
Av Åke Sjöholm, Stockholm.
Referat av artikeln:
Lee HC, Kim S-J, Kim K-S, Shin H-C, Yoon J-W. Remission in models of type 1 diabetes by gene therapy using a singlechain insulin analogue. Nature 2000; 408: 483-488 (kommentar sid 420-421).Patienter med insulinberoende typ-1 diabetes får vidkännas betydande inskränkningar i sin livsstil, som präglas av dagliga insulininjektioner, livslång blodsockermonitorering och strikt kosthållning. Trots detta, uppträder organkomplikationer förr eller senare beroende på att de intermittenta insulininjektionerna inte motsvarar kroppens egna kontinuerliga insulinfrisättning som hos friska exakt balanserar blodsockernivån.
Ett alternativ för ett fåtal av dessa patienter har varit transplantation av hela pankreas, ett omfattande ingrepp som dock både är kirurgiskt komplicerat och förenat med hög mortalitet. Ett på senare år framtaget alternativ är att endast endokrina pankreas, dvs de Langerhanska cellöarna, transplanteras, en procedur som visserligen är betydligt mindre invasiv men som hittills tyvärr uppvisat påfallande dåliga resultat
- endast 8 procent är insulinfria efter ett år.
till toppenBanbrytande
I en banbrytande artikel, som publiceras i veckans utgåva av Nature, har man använt sig av sinnrika och sofistikerade metoder för att med genterapi stadigvarande bota experimentell typ-1 diabetes i två olika djurmodeller för denna sjukdom, dels streptozotocin-inducerad diabetes och dels den genetiskt spontandiabetiska NOD-musen. Tidigare försök med genterapi har varit måttligt framgångsrika.
Finessen i denna studie är dels att man valt att inducera ett artificiellt uttryck av en okomplicerad insulinanalog i levern och dels att man konstruerat genhybriden så att dess uttryck står under kontroll av en promotorregion reglerad av glukos (leverns enzym pyruvatkinas).
till toppenProblem tidigare
Tidigare försök med ektopiskt insulinuttryck har mött svårigheter pga att proinsulinmolekylen, som endast uppvisar 1-2 % av insulinets biologiska aktivitet, måste klyvas och processas proteolytiskt intracellulärt innan slutprodukten (färdigt insulin) kan släppas ut i blodet. De enzymer som krävs för denna komplexa process finns i stort sett endast i pankreas’ beta-celler.
I studien har man genialiskt nog undvikit denna problematik genom att syntetisera en enkelkedjig insulinanalog som, trots att den endast består av 7 aminosyror, uppvisar 20-40 % av insulinets biologiska aktivitet.Således krävs ingen proteolytisk klyvning, som ju är fallet hos ordinärt insulin. Denna genhybrid placerades i ett modifierat virus som injicerades i vena porta och således hamnade i levern. Faktiskt visade det sig också att det virala genomet endast uttrycktes i levern.
Ett annat betydande problem med artificiellt insulinuttryck har varit svårigheterna att få detta att exakt matcha rådande blodsockernivåer. I artikeln i Nature, har man snillrikt nog löst detta genom att placera uttrycket av insulinanalog-genen under kontroll av en glukoskänslig promotorregion, nämligen leverenzymet pyruvatkinas, som således känner av blodsockret och styr insulinfrisättningen därefter.
till toppenGoda resultat
Genom dessa genialiska tekniker, lyckades man åstadkomma en normal blodsockerprofil under hela försöksperioden som uppgick till 8 månader. Trots en något förlångsammad frisättning av insulinanalogen (jämfört med den snabba exocytosprocessen i pankreas) lyckades de virustransfekterade djuren bibehålla såväl fasteblodsocker som postprandiella glukosnivåer som i det närmaste liknade friska djur. Huruvida denna approach kan användas hos patienter med typ-1 diabetes är dock inte självklart. Den humana levern har betydligt lägre basal glukosproduktion än råttor och möss.Om insulinanalogen ska uttryckas i levern, kan hepatocyterna komma att utsättas för extremt höga lokala nivåer av insulin. Vad medför detta? Ingen vet. Långdragen hypoglykemi, speciellt postprandiell sådan, är ett annat potentiellt problem vid irreversibel insulinproduktion även om detta inte noterades i försöksdjuren. Återigen kan man dock fråga sig hur människan reagerar. Icke desto mindre är konceptet med en glukoskänslig promotor högintressant och kan tänkas minimera problematiken med hypoglykemier även om andra faktorer som normalt reglerar insulinbehovet in vivo (t.ex. kostvanor förutom glukos, kropps-vikt, perifer insulinresistens, ålder, tillväxtfaser såsom pubertet och graviditet etc) säkerligen kräver än mer sofistikerade och avancerade metoder än så.
Åke Sjöholm, docent
Karolinska sjukhuset, Solna
E-post: Ake@crch.hawaii.eduObesity linked with increases
in type 2 diabetes and
healthcare costs
Från Medical Reuters.
Reuters Health US SurgeonGeneral David Satcher issued a ”very serious wake-up call” to Americans on the problem of obesity, saying that ”dramatic increases” in the number of overweight and obese adults and children in the 1990s have led to a 30% increase in type II diabetes. Addressing a gathering of physicians, scientists, and policy-makers at the Institute of Medicine’s 30th Annual Meeting, Dr. Satcher said physicians are now seeing children as young as 10 years old with this disease, something that was nearly unheard of a decade ago. Obesity also is associated with an increased risk of hypertension, cardiac disease, cancer, complications in pregnancy and early death, he noted.
Reversing the trend, Dr. Satcher said, will require a concerted effort on the part of private and public health officials, educators, and the food industry, similar to the country’s anti-smoking campaign. According to the latest federal government statistics,54.9% of US adults are overweight, and 22.3% are obese. More men than women are overweight (51 million versus 47 million), but among those who are overweight, women are more likely than men to become obese. Among African-American women, 40% are obese, Dr. Satcher said. Besides the healthrelated complications of obesity, the cost in healthcare dollars is considerable, Dr. F. Xavier Pi-Sunyer of Columbia University reported.
The total comes to roughly $100 billion in direct and indirect costs, he said. Indirect costs include 39 million missed work days, 239 million days of restricted activity, and 889 million bed days. Americans spend another $33 billion on weight-loss aids, such as diet pills and self-help books, Dr. Pi-Sunyer said. While genetics may predispose some people to obesity, experts are looking more at environmental factors such as fast-food consumption and physical inactivity as a cause of the current crisis and as a signal point for public health interventions.
According to Dr. Kelly Brownell of Yale University in New Haven, Connecticut, more than 5000 schools in the US have agreements with fast-food franchises to provide school meals. Moreover, Americans are exposed to an estimated 10,000 television food ads, many of them promoting high-fat choices. Dr. Brownell recommends banning fast foods and soft drinks from schools, regulating TV ads that are aimed at children, and subsidizing the sale of healthy foods at the national level to bring down the costs of fruits and vegetables. He also proposes, if needed, imposing a tax on ”poor foods” to help realize the other four goals.
IOM meeting attendees also focused on new research on the role of the energy density of foods in dietary control. ”This is the big news in this field,” according to Dr. Barbara Rolls, a nutritionist at Pennsylvania State University. ”Small reductions in the energy density of one’s diet can lead to significant and spontaneous decreases in energy intake,” without lowering one’s overall caloric intake, she explained.
In general, high-fat foods raise the energy density of a meal, while water and fiber lower it. So, for example, a person could eat a larger helping of pasta mixed with vegetables, and thus be more satiated than by eating pasta alone—without adding any calories.
The bottom line, Dr. Satcher said, is prevention through healthier lifestyles, early education, and regular physical activity—30 minutes a day, five times a week, as recommended by the Healthy People 2010 initiative. ”This country is penny-wise and pound-foolish when it comes to investment in prevention,” Dr. Satcher said, calling for a research agenda that ”balances health promotion, disease prevention, early detection, and universal access to healthcare.”Red
NPH x 2 daily beats
ultralente x 1 in type 2
Från Diabetes Care 2000;23:1612-1618.Twice-daily injections of NPH insulin provide better results in type 2 diabetes than do once-daily injections of ultralente insulin, according to a report in the November issue of Diabetes Care.
Dr. Roy Taylor, from the Diabetes Center in Newcastle upon Tyne, UK, and colleagues compared the two regimens in a crossover study of 79 patients with type 2 diabetes. NPH insulin lowered hemoglobin A1c (HbA1c) levels from 11.4 to 9.0 mmol/L, the authors report, better than the reduction to 9.7 mmol/L achieved with ultralente insulin. The crossover from NPH insulin to ultralente insulin brought a worsening of HbA1c, whereas the crossover from ultralente insulin to NPH insulin brought a significant improvement.
Ultralente insulin was associated with 14 hypoglycemic episodes requiring outside assistance compared with one associated with NPH insulin, despite similar fasting blood glucose levels with the two treatments. Overall hypoglycemia rates were 6.0 per patient-year for ultralente insulin and 4.7 per patient-year for NPH insulin. Patient satisfaction with treatment rose with the initiation of insulin therapy, and NPH insulin brought significantly higher increases in patient satisfaction than did ultralente insulin.
”Patients are sometimes unkeen at the idea [of insulin therapy],” Dr. Roy acknowledged in comments to Reuters Health. ”I strike a deal with them, offering to stop the insulin after 2 months if they wish. Ninety-nine percent of people would not dream of stopping insulin at that stage because they have discovered their full energy levels and enjoyment of life again.”Red
Tight metabolic control in diabetic
pregnancy necessary for normal fetal
growth
Från Diabetes Care 2000;23:1494-1498.Maintenance of physiologically normal glucose levels in both the second and third trimesters of pregnancy is critical to avoid alterations in fetal growth in pregnant women with type 1 diabetes, according to a report in the October issue of Diabetes Care.
Dr. Giorgio Mello, and colleagues at the University of Florence, in Italy, examined the effects of maternal metabolic control on fetal growth in 98 diabetic women with singleton pregnancies. They divided the women into three groups based on the degree of metabolic control achieved during the second and third trimesters of pregnancy: daily glucose level at or below 95 mg/dL for both trimesters; daily glucose level above 95 mg/dL during the second trimester but at or below this level during the third trimester; and daily glucose above 95 mg/dL during both trimesters.
Only the infants of women in the first group, who achieved
normal daily glucose levels throughout the entire last two trimesters of pregnancy, had birth weight and other anthropometric parameters similar to controls. By comparison, the infants of women with less successful metabolic control were significantly more likely to be large-for-gestational-age, had greater mean ponderal indexes and thoracic circumferences, and had significantly smaller cranial/thoracic circumference ratios than control infants.
”What should be stressed from the results of our study is that there seems to be a continuous relationship between maternal glucose levels and infant birth weight,” Dr. Mello and his team say. ”The effect of only marginally higher than physiological glucose values on offspring is notable.” With this in mind, the investigators stress ”that it is not sufficient to achieve near-normal glucose values in diabetic pregnancies.” Rather, the goal should be to achieve daily glucose levels at or below 95 mg/dL ”as early as the second trimester” and maintain these levels throughout the rest of the pregnancy.Red
Lipid-carbohydrate interactions in
reduced muscle insulin sensitivity
- Another look at the Randle Cycle
Från International Journal of Metabolism 8 December 2000.In the early 1960s, Randle (1) developed a paradigm that was to give rise to numerous studies. When a muscle switches from using glucose to fatty acids as an energy source during fasting for instance, the predominance of fatty-acid oxidation blocks the glycolytic pathway through the accumulation of acetyl CoA and citrate, which inhibits pyruvate dehydrogenase and phosphofructokinase, respectively. This blocking action leads to the accumulation, upstream, of glucose-6-phosphate, inhibition of hexokinase, and reduced uptake and oxidation of glucose.
Although the existence of this glucose-fatty acid interaction has been confirmed in vivo in healthy subjects and in situations of reduced insulin sensitivity such as obesity and type 2 diabetes. During the past 10 years, a number of studies have shown that increased oxidation of fatty acids is not involved in the reduction of muscle insulin sensitivity (2). In fact, oxidation of glucose is increased, and that of fatty acids is reduced, in patients with type 2 diabetes (3), and in obese subjects (4), in postabsorptive situations, compared with insulin-sensitive control subjects. The increased oxidation of glucose is negatively correlated with insulin sensitivity (4).
In a situation of stimulation by insulin, during euglycemic and hyperinsulinemic clamp studies, muscle in subjects with reduced insulin sensitivity displays a ”metabolic rigidity”. Neither oxidation of glucose nor that of fatty acids is significantly changed, whereas in normal subjects oxidation of glucose increased and that of fatty acids decreased (3-4).
The triglyceride content of muscle is increased in situations of reduced insulin sensitivity, and correlated with the severity of the reduction (2). The data strongly suggest tht accumulation of triglycerides in muscle results from decreased oxidation and from an increase in the esterification of fatty acids.
The increased musle content of malonyl-CoA observed in animal models of insulin resistance (5) is seen to be involved in the mechanism leading to reduced oxidation of fatty acids and the accumulation of triglycerides.
Malonyl-CoA inhibits carnitine palmitoyl tranferase (CPT). CPT activity is, in fact, reduced in the muscle of obese subjects with reduced insulin sensitivity (2, 6). The reduced CPT activity results in reduced oxidation metabolism in the mitochondria. Among other things, this relate to oxidation of fatty acids, but glucose metabolism may also be affected (2, 7).
In addition, the resulting accumulation of long-chain acyl-CoA can have an adverse effect on the insulin receptor signalling network by activating protein kinase C thorugh diacylglycerol. This kinase is itself able to inactivate the insulin receptor and its substrates, by phophorylating some of their serine residues (2). Ceramide (a sphingolipid derivative of palmitate, and thus another fatty acid derivative) inhibits the insulin stimulation of protein kinase B (8), The accumulation of lipids in muscle is this liable to inhibit the action of insulin in a number of ways.
All of these data show that, in situation of reduced insulin sensitivity, the interaction between lipids and carbohydrates in muscle go beyond the initial paradigm of the glucose-fatty acid ”cycle”. In type 2 diabetes and obesity, lipotoxicity is involved in the reduction of muscle insulin sensitivity, through mechanisms that favor the esterification of lipids rather than oxidatation.P. Freychet, Nice, France
References
1. Randle et al. Lancet 1963;1:785- 789
2. Kelley et al, Diabetes 2000;49:677-683
3. Kelley et al, J Clin Invest 1990;86:1999-2007
4. Kelley et al Am J Physiol 1999;277:E1130.E1141
5. Ruderman et al, Am J Physiol 1999;276:E1-E18.
6. Simoneau et al, FASEB J 1999;13:2051-2060
7. Pendergrass M et al, Diabetes 1998;47:387-394
8. Schmitz-Pfeiffer C et al, J Biol Chem 1999;274:24202-24210Distal pancreatectomy increases risk for
diabetes in pancreatitis patients
Från Gastroenterology 2000;119:1324-1332.Of all elective pancreatic surgical procedures, only distal pancreatectomy appears to increase the risk for diabetes mellitus in patients with chronic pancreatitis, according to a report by French researchers.
Dr. David Malka and colleagues, from Hopital Beaujon, Clichy, France, collected data on 500 patients with chronic pancreatitis. Over the mean follow-up period of 7 years, the researchers compared outcomes for the 231 patients who underwent elective pancreatic surgery with the 222 who never had surgery.
According to the team’s report in the November issue of Gastroenterology, the mean cumulative rate of diabetes mellitus was 83% at 25 years after onset of pancreatitis. While the prevalence of diabetes was not greater overall in the group that underwent surgery, it was higher 5 years after distal pancreatectomy (57%), compared with ”pancreaticoduodenectomy (36%), pancreatic drainage (36%), or cystic, biliary, or digestive drainage (24%).”
Further, the investigators say that ”distal pancreatectomy (risk ratio, 2.4) and early onset of pancreatic calcifications (risk ratio, 3.2) were the only independent risk factors for diabetes mellitus.” Dr. Malka and colleagues also note that pancreatic drainage did not prevent the onset of diabetes. They say that ”this finding does not support prophylactic pancreatic drainage procedures performed early in the course of chronic pancreatitis as a means of preventing the progression of endocrine pancreatic insufficiency.” It is the progression of chronic pancreatitis, they say, that ”seems to be the main determinant of diabetes mellitus in both surgical and nonsurgical patients.”Red
Blood glucose levels have prognostic
value in acute pancreatitis
Från American and International Association of Pancreatology och Medical Reuters.CHICAGO (Reuters Health) - The results of a prospective study conducted at three international medical centers indicate blood glucose levels are of prognostic value in patients with acute pancreatitis. The findings were reported here by a multicenter team at a meeting of the American and International Association of Pancreatology.
Headed by Dr P. G. Lank-isch, of the Municipal Clinic of Luneburg, Germany, the study included 218 nondiabetic patients (133 males and 85 females) with a first attack of acute pancreatitis. The subjects all underwent CT scanning within 72 hours of admission to determine presence of pancreatitis. A blood glucose level above 125 mg/dL was considered abnormal.
Severity of pancreatitis was assessed by initial organ failure, serum creatinine greater than 2.0 mg/dl after rehydration, need for artificial ventilation and/or dialysis, surgery and other parameters. Ninety patients (41%) had a normal blood glucose level and 128 patients (59%) had an abnormal blood glucose level on admission. They found that high blood glucose on admission was significantly associated with the need for artificial ventilation, a high Balthazar score, which indicated necrotizing pancreatitis, a longer hospital stay, and the development of a pancreatic pseudocyst.
Dr. Lankisch’s group concludes that ”a simple inexpensive measurement of blood glucose level on hospital admission in a nondiabetic patient with acute pancreatitis is a very helpful assay for assessing the prognosis of the disease.”Red
High TG in diabetic women
threaten outcome of ACB
Från Diabetes Care 2000;23:1648-1653.Preoperative hypertriglyceridemia in women with diabetes mellitus undergoing coronary artery bypass graft surgery (CABG) is associated with increased late mortality and cardiac event risk, report investigators from the Cleveland Clinic Foundation. The effect in men is much less marked, according to Dr. Dennis L.
Sprecher and associates.
”When it comes to patients who already have severe disease, post-CABG patients, I was stunned by the distinct difference between genders,” Dr. Sprecher told Reuters Health. The longitudinal study included 792 men and 380 women with diabetes mellitus who underwent CABG between 1982 and 1992. As reported in the November issue of Diabetes Care, the researchers observed no significant difference between men and women with normal triglyceride levels for overall survival or event-free survival. However, a significant triglyceride effect was observed in women after the first 3 years, with hazard ratios of 1.89 for mortality and 1.49 for myocardial infarction (MI), revascularization, or death, for those with upper-quartile triglyceride values compared with the other women. The corresponding hazard ratios for men were 1.02 and 1.28.
”A lot of people feel that triglycerides are a surrogate for insulin resistance in diabetes,” Dr. Sprecher noted. ”We presented the Diabetes Care paper to discriminate specifically [between] the triglycerides and diabetes issue, and I think it was successful in saying that each one of these adds more fuel to the fire.” Dr. Sprecher and Gregory L. Pearce recently presented related data (see Reuters Health report, October 2), showing that women with metabolic coronary risk factors are at significantly increased risk following CABG. ”Is it possible that the end game of mortality...may have a different nurture within a female than in a male?” Dr. Sprecher mused. ”Plaques still develop in men, but they don’t necessarily result in a rupture/MI/death paradigm.”
”Therefore the female seems more prone to the mortality,” he added. ”Maybe they have smaller coronary vessels. Or perhaps there is an endocrine physiology in which a toxicity to vessels combines [with diabetes and hypertriglyceridemia] in a woman to make this very deleterious.” In recommending treatment for women with diabetes and high triglycerides prior to CABG, Dr. Sprecher said, ”The relatively less sophisticated strategy is that you lower triglyceride levels, and that may be relevant. At the very least, however, I think that in a diabetic patient you have to take all risk factors and control them very carefully.”Red
Diabetics on orlistat can lose less weight
than nondiabetics to reduce CVD risk
Från IDF november 2000 i Mexico City.Compared with their nondiabetic counterparts, obese patients with type 2 diabetes treated with the lipase inhibitor orlistat do not need to lose as much weight in order to reduce the risk of cardiovascular disease.
In a substudy of the Framingham Heart Study, Dr. Peter W. F. Wilson of Boston University and colleagues randomized 11,074 obese diabetic and nondiabetic patients to receive either orlistat 120 mg t.i.d. or placebo for a year. The nondiabetics had at least one risk factor for heart disease other than obesity. All subjects also followed a restricted-calorie diet. The objective was to determine how much weight loss was necessary to reduce cardiovascular disease risk, Dr. Wilson commented. Mean body mass index in the study group was 35. At baseline, the estimated risk of coronary heart disease at 10 years was 15.5% for diabetics on orlistat and 15.7% for diabetics on placebo, compared with 6.5% and 6.6% for nondiabetics, respectively.
Orlistat induced significantly greater weight loss in all recipients than placebo, but diabetics lost less weight than nondiabetics in the active treatment arm. CVD risk reduction with orlistat was 18% after 1 year in diabetics compared with a risk reduction of 19% in nondiabetics on orlistat, which was roughly equivalent, according to the researchers. Risk reduction in diabetics on placebo was 4% and it was 11% in nondiabetics on placebo.
The primary finding, Dr. Wilson pointed out, was that although risk reduction was similar in both groups on orlistat, it was achieved with 40% less weight loss in the diabetics. ”Small changes in weight—5 to 10 pounds—are enough to reduce risk” in diabetics, Dr. Wilson commented. In both groups, he said, the specific lipid-lowering effect of the drug, a gastrointestinal lipase inhibitor, may account for the greater lowering in CVD risk than that achieved by weight loss alone.Red
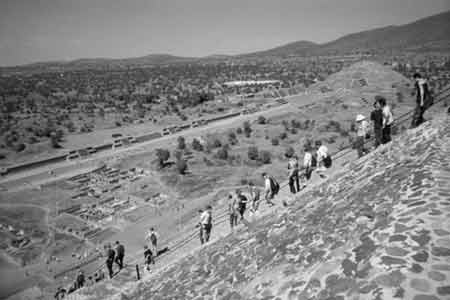
Mexico november 2000: Sol- och månpyramiderna strax norr om Mexico City